Introduction
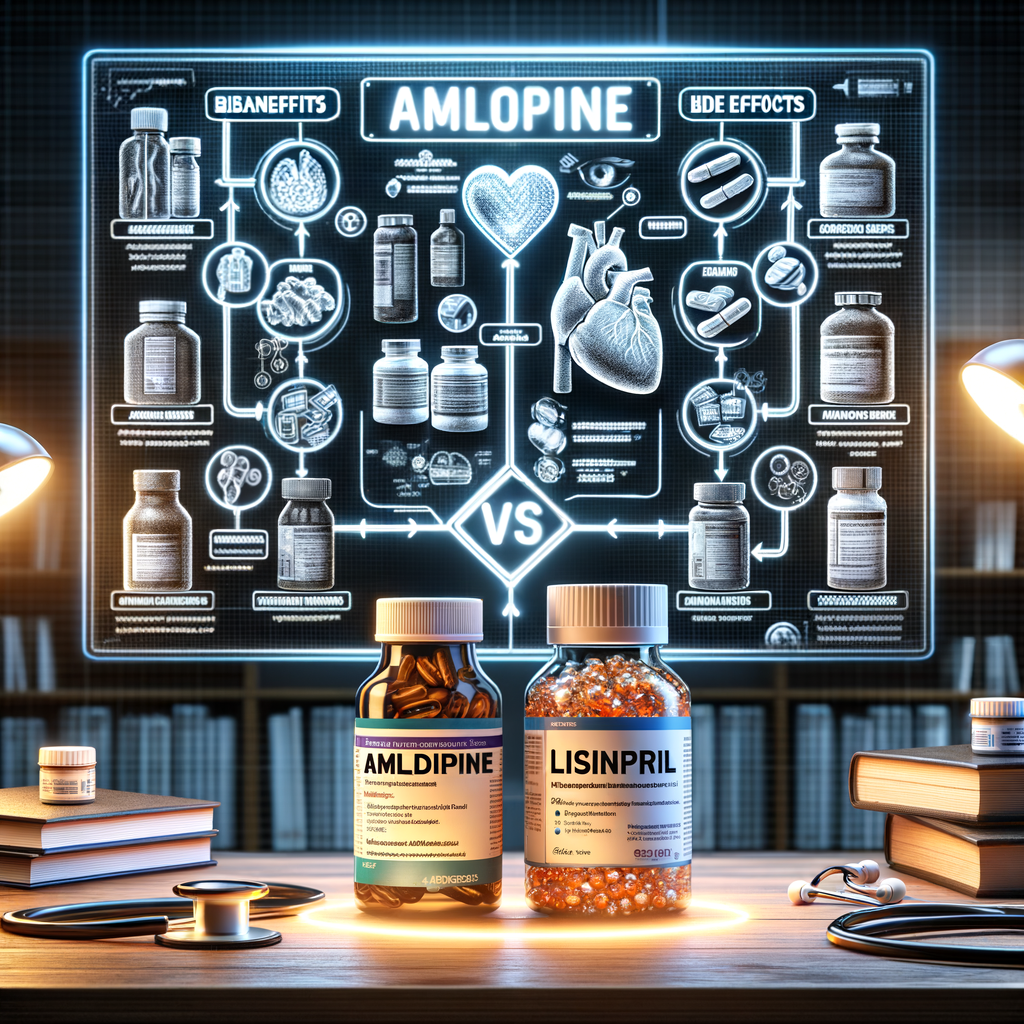
Choosing the right blood pressure medicine can feel overwhelming. You likely saw the names Amlodipine and Lisinopril and wondered which suits you best. This guide helps you weigh benefits, risks, and real-world factors. You will get clear, practical advice that fits common situations.
I wrote this piece to be reader-friendly and evidence-based. I focus on differences that matter for your health. In the end, you should feel ready to talk with your clinician and ask the right questions.
What Amlodipine and Lisinopril Are
H2: What is Amlodipine?
Amlodipine belongs to a class called dihydropyridine calcium channel blockers. It relaxes blood vessels by blocking calcium entry into muscle cells. As a result, it lowers blood pressure and eases strain on the heart.
Doctors often prescribe amlodipine for high blood pressure and angina. It works steadily and usually requires one daily dose. Side effects can include swelling, flushing, and fatigue.
H2: What is Lisinopril?
Lisinopril is an ACE inhibitor, or angiotensin-converting enzyme inhibitor. It reduces the production of angiotensin II, a hormone that narrows blood vessels. That leads to vessel relaxation and lower blood pressure.
Clinicians use lisinopril for hypertension, heart failure, and kidney protection in diabetes. It typically starts at a low dose and can increase as needed. Common side effects include cough and elevated potassium.
Key Differences at a Glance
H2: Major Differences Between Amlodipine vs Lisinopril
Both drugs lower blood pressure. Yet they act on different systems in the body. Amlodipine targets calcium channels in vessel muscle. Lisinopril blocks an enzyme in the renin-angiotensin system.
Therefore, their typical side effects and clinical uses vary. For instance, amlodipine often causes peripheral swelling. Lisinopril can cause a persistent dry cough or rare angioedema. Also, lisinopril affects kidney function and potassium more than amlodipine.
Below is a quick comparison table to help you see the differences immediately.
H3: Quick Comparison Table
– Drug class: Amlodipine — Calcium channel blocker | Lisinopril — ACE inhibitor
– Typical use: Amlodipine — Hypertension, angina | Lisinopril — Hypertension, heart failure, kidney protection
– Common side effects: Amlodipine — Edema, flushing | Lisinopril — Cough, hyperkalemia
– Dosing: Amlodipine — Once daily (2.5–10 mg) | Lisinopril — Once daily (5–40 mg)
– Pregnancy category: Amlodipine — Use with caution | Lisinopril — Contraindicated in pregnancy
– Kidney effects: Amlodipine — Minimal direct effect | Lisinopril — Affects renal hemodynamics
Clinical Uses and Evidence
H2: When Doctors Prefer Amlodipine
Clinicians often choose amlodipine for patients with isolated high blood pressure or chest pain. It lowers systolic pressure effectively in older adults. Also, it proves useful in people with peripheral vascular disease.
Because it relaxes coronary arteries, amlodipine helps prevent angina attacks. Additionally, it does not typically change potassium levels or harm kidneys directly. Therefore, doctors may prefer it in patients with chronic kidney disease who need blood pressure control without altering renal function.
H2: When Doctors Prefer Lisinopril
Lisinopril shines when patients have heart failure or diabetic kidney disease. It lowers mortality in heart failure and slows kidney damage progression in diabetes. Many guidelines recommend ACE inhibitors as first-line therapy for these conditions.
Furthermore, clinicians often choose lisinopril for younger patients with hypertension who can tolerate it. It offers strong protection against stroke and heart attack when combined with other agents. However, doctors avoid lisinopril in pregnancy and in people with previous angioedema from ACE inhibitors.
Mechanism of Action
H2: How Amlodipine Works
Amlodipine blocks L-type calcium channels in vascular smooth muscle. This action prevents calcium from entering cells. Consequently, the muscle relaxes and the vessel dilates.
As vessels dilate, resistance falls and blood pressure declines. The drug works slowly, so blood pressure control remains steady over 24 hours. You usually do not feel dramatic shifts in blood pressure.
H2: How Lisinopril Works
Lisinopril inhibits the angiotensin-converting enzyme. That lowers angiotensin II production, a potent vasoconstrictor. As a result, vessels relax and blood pressure drops.
Additionally, ACE inhibition reduces aldosterone release. Lower aldosterone decreases sodium and water retention. Therefore, lisinopril can reduce blood volume and ease heart workload.
Efficacy and Blood Pressure Control
H2: Comparing Blood Pressure Lowering
Both medications lower blood pressure effectively. Studies show similar average reductions in systolic and diastolic pressure when doses are comparable. Yet individual responses vary widely.
Some patients respond better to a calcium channel blocker. Others show greater benefit with an ACE inhibitor. In practice, clinicians may start one drug and switch if control remains inadequate.
H2: Combination Therapy
Often, clinicians use both agents together for tougher cases. Combining amlodipine with lisinopril can provide additive effects. The drugs act on different pathways, so they complement each other.
However, combining increases the risk of side effects. For example, you might see more dizziness or low blood pressure. Therefore, clinicians monitor patients closely after starting combination therapy.
Dosing and Administration
H2: Amlodipine Dosing Basics
Amlodipine typically starts at 2.5–5 mg once daily. Most adults take 5–10 mg per day based on response. Seniors or those with liver problems often start lower.
You can take amlodipine with or without food. Take it at about the same time each day. Do not stop suddenly; consult your doctor before stopping.
H2: Lisinopril Dosing Basics
Doctors usually start lisinopril at 5–10 mg once daily. Typical maintenance ranges from 10 to 40 mg once daily. The dose depends on blood pressure response and kidney function.
Take lisinopril at the same time each day. You can take it with or without food. Monitor your blood pressure and labs as directed.
Side Effects and Safety
H2: Common Side Effects of Amlodipine
Amlodipine often causes ankle swelling, especially at higher doses. You might also feel flushing, palpitations, or mild dizziness. These effects tend to be dose-related.
Usually, swelling reduces if doctors lower the dose. In many cases, it remains tolerable and does not require stopping the drug. Still, mention any troubling symptoms to your clinician.
H2: Common Side Effects of Lisinopril
Lisinopril frequently causes a dry cough in some patients. This cough often resolves after stopping the drug. Less commonly, lisinopril can cause elevated potassium or reduced kidney function.
A rare but serious effect is angioedema. Angioedema causes rapid swelling of the face, lips, or throat. Seek immediate medical care if this happens.
H3: Serious Adverse Effects and Monitoring
Both drugs require monitoring under certain conditions. Amlodipine lowers blood pressure and may cause lightheadedness if you stand up quickly. Lisinopril requires monitoring of kidney function and potassium, especially when combined with diuretics or potassium supplements.
Additionally, stop lisinopril before planned pregnancy and notify your doctor if you become pregnant. Both drugs should be used cautiously in patients with low blood pressure or severe cardiac issues.
Who Should Avoid Each Drug
H2: When to Avoid Amlodipine
Avoid amlodipine if you have worsening heart failure with low blood pressure. Also, be cautious in people with significant liver impairment. If you experienced a severe allergic reaction previously, skip it.
If you develop severe swelling or troublesome side effects, consult your clinician. They may recommend an alternative medication.
H2: When to Avoid Lisinopril
Do not use lisinopril during pregnancy. It causes serious fetal harm. Also avoid it if you have a history of angioedema with ACE inhibitors.
If you have bilateral renal artery stenosis, lisinopril may worsen kidney function. Moreover, avoid using lisinopril with high potassium levels or certain potassium-sparing drugs unless closely monitored.
Special Populations
H2: Use in Older Adults
Older adults often respond well to amlodipine. It reduces systolic blood pressure effectively. However, it can cause more peripheral edema in this group.
Lisinopril also works in older adults but requires careful monitoring. Older people often have reduced kidney function. Therefore, clinicians check creatinine and potassium more often.
H2: Use in People with Diabetes or Kidney Disease
Lisinopril provides kidney protection in many patients with diabetes. It reduces proteinuria and slows kidney disease progression. As a result, clinicians often prefer ACE inhibitors for this group.
Yet if kidney function falls or potassium rises, doctors may switch to a different drug. Amlodipine does not offer the same kidney-protective benefits, but it does effectively lower blood pressure without affecting potassium.
H2: Use in Pregnancy and Breastfeeding
Avoid lisinopril during pregnancy because it harms the fetus. If you plan pregnancy, your clinician will change your medication. Amlodipine remains an option in pregnancy only when benefits outweigh risks.
Both drugs appear in breast milk to varying degrees. Discuss breastfeeding plans with your clinician before choosing therapy.
Drug Interactions
H2: Important Interactions with Amlodipine
Amlodipine interacts with strong CYP3A4 inhibitors and inducers. Drugs like clarithromycin may increase amlodipine levels. Conversely, rifampin can lower its effect.
Also, combining amlodipine with other blood pressure medications can cause low blood pressure. Monitor closely when combining classes.
H2: Important Interactions with Lisinopril
Lisinopril interacts with potassium supplements and potassium-sparing diuretics. Combining them may raise serum potassium. Also, NSAIDs can blunt its effect and harm kidneys, especially in older adults.
Combining lisinopril with diuretics can cause a sudden drop in blood pressure. Always consult your clinician before adding or stopping any medication.
Cost and Accessibility
H2: Generic Availability and Cost
Both amlodipine and lisinopril are available as generics. This availability keeps costs low for most patients. Insurance plans typically cover both drugs.
If cost remains a barrier, clinicians can prescribe generic options or adjust the regimen. Community clinics and pharmacies may also offer discount programs.
H2: Brand Names and Formulations
Amlodipine appears under brand names such as Norvasc. Lisinopril appears as Prinivil or Zestril. Various pills and combination tablets exist for both drugs.
Combination pills pair lisinopril with diuretics or amlodipine with other agents. These options can simplify dosing and improve adherence.
Making the Choice: Factors to Consider
H2: Clinical Factors to Guide Choice
Start by considering your medical history. If you have diabetes or heart failure, lisinopril might offer added benefits. If you have angina or peripheral vascular disease, amlodipine may work better.
Also weigh side effects you can tolerate. For instance, you might prefer to avoid a drug that causes cough. Discuss all allergies and prior drug reactions with your clinician.
H2: Lifestyle and Practical Factors
Consider lifestyle factors like adherence and cost. A once-daily pill supports better adherence. Both drugs generally require once-daily dosing, so they score well here.
Additionally, consider travel, pregnancy plans, and other medications you take. These practical issues often sway the decision.
H3: Shared Decision-Making with Your Clinician
Speak openly about your goals and concerns. Ask about expected benefits and risks in your case. Request clear plans for blood tests and follow-up.
Your clinician should explain why they recommend one drug over another. Together, you can balance short-term control and long-term protection.
Real-World Scenarios
H2: Scenario 1 — Older Adult with Isolated Systolic Hypertension
An older patient with systolic hypertension and leg swelling might benefit from amlodipine. It reduces systolic pressure effectively. Yet, if edema worsens, the clinician can switch or lower the dose.
Alternatively, combining low-dose amlodipine with a diuretic can minimize swelling. The clinician will monitor blood pressure and electrolytes.
H2: Scenario 2 — Middle-Aged Patient with Diabetes and Proteinuria
A patient with diabetes and rising urine protein likely benefits from lisinopril. Lisinopril can slow kidney damage and lower proteinuria. The clinician will monitor creatinine and potassium closely.
If kidney function declines, the clinician may adjust doses or consider alternatives.
H2: Scenario 3 — Young Person with Hypertension and Asthma
If a young person has hypertension and a strong cough history, they may avoid lisinopril. Amlodipine could work as the first-line option. If the patient suffers angina, amlodipine also benefits coronary circulation.
However, clinicians also consider lifestyle factors and adherence when choosing therapy.
Switching Between the Two Drugs
H2: How Clinicians Switch Safely
Doctors often switch when side effects occur or when the drug fails to control blood pressure. They may taper one and start the other the next day. Usually, they allow a washout only when switching from an ARB or ACE inhibitor to avoid overlap.
When switching, clinicians monitor blood pressure, kidney function, and electrolytes. They also watch for ankle swelling or cough developing after the change.
H2: Things to Watch For After Switching
Expect adjustments in blood pressure control in the first weeks. You might feel dizzy or lightheaded initially. Report severe symptoms, fainting, or rapid heartbeat immediately.
Also, labs may require recheck within 1–2 weeks with lisinopril. Your clinician will guide the monitoring schedule.
Lifestyle Tips to Boost Medication Effectiveness
H2: Diet and Sodium Reduction
Lowering sodium helps all blood pressure medicines work better. Aim for under 2,300 mg of sodium daily. Even small reductions can lower blood pressure significantly.
Eat more vegetables, fruits, and whole grains. Reduce processed foods and fast food intake. These changes complement medication effects.
H2: Exercise and Weight Management
Regular exercise helps control blood pressure and weight. Aim for 150 minutes of moderate exercise per week. Even brisk walking delivers benefits.
Losing 5–10% of body weight often lowers blood pressure. Combining medication with lifestyle changes gives the best results.
H2: Avoiding Alcohol and Tobacco
Limit alcohol intake to moderate levels or avoid it entirely. Smoking damages blood vessels and raises cardiovascular risk. Quitting smoking reduces heart attack and stroke risk over time.
Medication adherence also improves when you reduce alcohol and tobacco use.
Monitoring and Follow-Up
H2: Home Blood Pressure Monitoring
Measure blood pressure at home to track progress. Use a validated upper-arm cuff and sit quietly before measuring. Record readings and bring them to appointments.
Share patterns with your clinician, including morning and evening readings. Home monitoring helps tailor doses accurately.
H2: Lab and Clinical Follow-Up
If you take lisinopril, expect kidney and potassium checks within the first 1–2 weeks. For amlodipine, clinicians typically check blood pressure and symptoms in follow-up visits. They may also assess swelling and heart rate.
Regular visits help catch side effects early and guide dose changes.
Cost, Insurance, and Generic Options
H2: Insurance Coverage and Generic Drugs
Most insurance plans cover both drugs in generic form. Generics make long-term treatment affordable for many patients. If cost still burdens you, ask your clinician about alternatives.
Pharmacy discount cards and manufacturer programs also reduce out-of-pocket costs. Community clinics can connect patients to these resources.
H2: When Cost Dictates Choice
If you must choose based on cost alone, either drug can work. Both have inexpensive generic options that provide good control. However, prioritize clinical appropriateness over cost when possible.
If cost prevents filling a prescription, contact your clinician or pharmacist for help options.
Frequently Asked Questions (FAQs)
H2: FAQs — Amlodipine vs Lisinopril
H3: 1. Can I take amlodipine and lisinopril together?
Yes. Many clinicians combine them for better blood pressure control. They act on different pathways for additive effects. Monitor blood pressure and watch for side effects.
H3: 2. Which drug is safer for people with kidney disease?
Lisinopril can protect kidneys in diabetic kidney disease. However, it affects renal hemodynamics and potassium. Doctors monitor labs closely. Amlodipine has less direct effect on kidneys.
H3: 3. Which drug causes less swelling?
Amlodipine more commonly causes peripheral edema. Lisinopril rarely causes this type of swelling. If swelling occurs, clinicians may lower the amlodipine dose or switch therapy.
H3: 4. Can lisinopril cause a cough forever?
The cough typically resolves after stopping lisinopril. However, it may take days to weeks to disappear. If the cough persists, seek further evaluation.
H3: 5. Is one drug better for heart failure?
Lisinopril improves survival in heart failure with reduced ejection fraction. Clinicians commonly use ACE inhibitors as foundational therapy. Amlodipine may help symptoms but does not offer the same survival benefit.
H3: 6. Can pregnant people take amlodipine or lisinopril?
Avoid lisinopril during pregnancy due to fetal harm. Amlodipine remains a possible option only if benefits exceed risks. Always discuss pregnancy plans before starting therapy.
H3: 7. Do these drugs interact with vitamins or supplements?
Yes; lisinopril can interact (Incomplete: max_output_tokens)