- Introduction
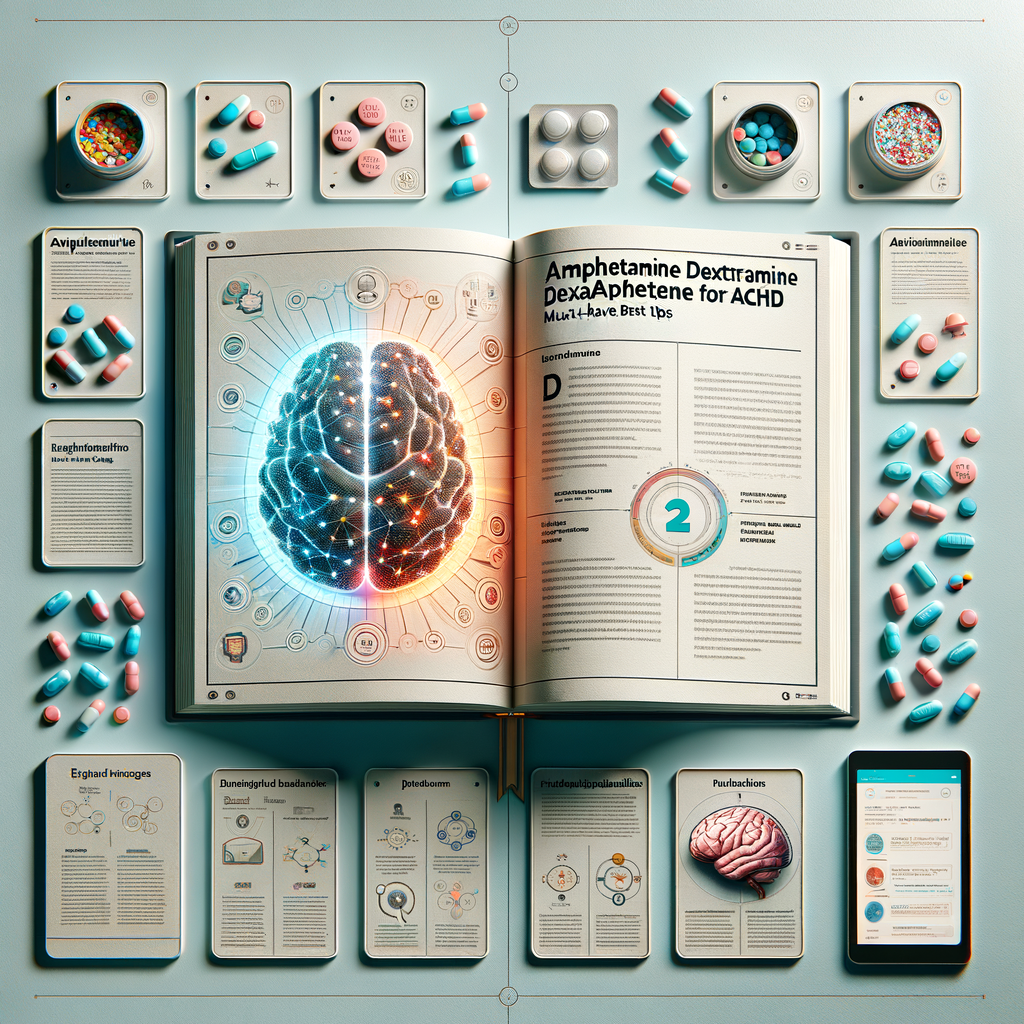
- What Is Amphetamine Dextroamphetamine?
- How It Differs From Other ADHD Medications
- How Amphetamine Dextroamphetamine Works
- Onset and Duration
- Common Benefits for People With ADHD
- Improved Executive Function
- Who Should Consider This Medication?
- Children, Teens, and Adults
- Dosage Forms and How to Choose
- Typical Dosing Strategies
- Maximizing Effectiveness: Practical Tips
- Nutrition and Timing
- Behavioral Strategies to Combine With Medication
- Side Effects: What to Expect
- Long-Term Considerations
- Drug Interactions and Precautions
- Medical Conditions That Require Caution
- Managing Common Problems
- Handling Missed Doses
- Misuse, Diversion, and Legal Issues
- Signs of Misuse
- Alternatives and Complementary Treatments
- When to Consider a Switch
- Special Populations: Children, Teens, Pregnant People, and Older Adults
- Monitoring and Follow-Up
- What to Report to Your Clinician
- Practical Tips for Parents and Caregivers
- School Strategies
- Cost, Insurance, and Access
- Pharmacy Tips
- Real-World Tips from Patients
- Safety During Travel and Special Situations
- When Treatment Fails to Work
- Key Takeaways
- Frequently Asked Questions (FAQs)
- Additional Questions You May Have
- References
Introduction
Amphetamine dextroamphetamine for ADHD has helped millions manage attention, impulsivity, and hyperactivity. Many people call these medications stimulants. Yet they act in a controlled and therapeutic way when used properly. In this article, I’ll explain how they work, when they help, and how to get the best results.
You’ll find practical tips, safety advice, and clear comparisons. I wrote this to help patients, caregivers, and anyone curious about treatment options. Also, I included a FAQ section to answer common questions that may not come up elsewhere.
What Is Amphetamine Dextroamphetamine?
Amphetamine dextroamphetamine is a combination of two active ingredients. It typically appears in brand names like Adderall. These medicines belong to a class called central nervous system stimulants.
They increase the levels of certain brain chemicals. Specifically, they boost dopamine and norepinephrine. Those changes help improve focus and reduce impulsive behavior. Doctors prescribe them most often for attention deficit hyperactivity disorder (ADHD).
How It Differs From Other ADHD Medications
Other ADHD meds include methylphenidate-based drugs. While similar, amphetamine dextroamphetamine and methylphenidate work slightly differently. For example, amphetamines tend to release stored neurotransmitters more strongly.
Furthermore, different people respond better to different drugs. That’s why clinicians try more than one option when needed. Also, the side effect profiles can differ, which influences choice.
How Amphetamine Dextroamphetamine Works
The drug increases dopamine and norepinephrine in the brain. Dopamine improves reward and motivation. Norepinephrine helps with attention and alertness.
It does this by blocking reuptake and promoting release of these neurotransmitters. Consequently, neural circuits involved in focus and executive function work better. That change reduces core ADHD symptoms.
Onset and Duration
Immediate-release forms start working within 30 to 60 minutes. Effects often last four to six hours. Extended-release versions can last up to 12 hours.
So, patients choose formulas depending on daily needs. For example, long-acting forms help cover a full school or work day. Short-acting forms work well for flexible dosing.
Common Benefits for People With ADHD
First, amphetamine dextroamphetamine improves attention. Many users report better concentration on tasks. They also find it easier to complete work and follow conversations.
Second, it reduces impulsivity and hyperactivity. People act more calmly and think before speaking. Together, these effects can improve school, work, and social outcomes.
Improved Executive Function
Executive functions include planning, organizing, and task switching. Patients often notice gains in these areas. Those gains lead to better time management and fewer missed deadlines.
Additionally, mood and motivation often improve indirectly. When ADHD symptoms fall, people feel more capable and confident.
Who Should Consider This Medication?
Doctors recommend amphetamine dextroamphetamine for diagnosed ADHD. A formal diagnosis usually involves history, rating scales, and sometimes testing. Clinicians assess symptoms across settings, such as school and home.
People with co-existing conditions need careful evaluation. Conditions like anxiety, bipolar disorder, and heart disease may affect treatment choice. Always discuss full medical history with your prescriber.
Children, Teens, and Adults
Healthcare providers prescribe this medication across ages. Children receive doses based on weight and response. Teens and adults often start at low doses and adjust upward.
Monitoring remains critical in all ages. Growth, sleep, mood, and blood pressure all require periodic checks. Families should keep open communication with the care team.
Dosage Forms and How to Choose
Amphetamine dextroamphetamine comes in immediate-release (IR) and extended-release (XR) forms. IR tablets release the drug quickly. XR capsules release it over many hours.
Below is a simple comparison table.
| Form | Onset | Duration | Best For |
|---|---|---|---|
| Immediate-Release (IR) | 30–60 minutes | 4–6 hours | Flexible dosing; short tasks |
| Extended-Release (XR) | 30–60 minutes | 8–12 hours | Full day coverage; school/work |
Discuss lifestyle and schedule with your clinician. That helps determine the right form. Also, consider side effects and daily routine.
Typical Dosing Strategies
Clinicians start with low doses. They then increase slowly to balance benefits and side effects. For kids, weight-based dosing often applies. For adults, clinicians use standard titration.
Some people split doses with IR forms. Others use a single XR dose in the morning. Work with your prescriber to find the right plan.
Maximizing Effectiveness: Practical Tips
Take medication at the same time each day. That consistency stabilizes blood levels. Also, take XR versions in the morning to avoid insomnia.
Maintain a healthy sleep routine. Stimulants can interfere with sleep for some people. Therefore, good sleep hygiene boosts medication benefits.
Nutrition and Timing
Certain foods affect absorption. For instance, acidic foods and vitamin C can reduce absorption. Conversely, a light breakfast often helps. Avoid large, fatty meals right before dosing.
Drink water and stay hydrated. Dehydration can intensify side effects like jitteriness. Also, regular meals help prevent appetite loss from becoming severe.
Behavioral Strategies to Combine With Medication
Medication works best with behavioral supports. Use planning tools, reminders, and lists. Break tasks into small steps and reward completion.
Therapies like cognitive behavioral therapy (CBT) help improve skills. Likewise, parent training can support children’s routines. Combining strategies gives the best long-term outcomes.
Side Effects: What to Expect
Common side effects include decreased appetite, dry mouth, and trouble sleeping. Some people feel jittery or nervous. Headaches and stomach upset also occur.
Most side effects are mild and fade as the body adapts. Yet some problems require attention. If you notice chest pain, shortness of breath, or severe mood changes, seek emergency care.
Long-Term Considerations
Long-term stimulant use needs periodic evaluation. Doctors monitor blood pressure, heart rate, and weight. In children, growth should be checked regularly.
Concerns about dependence exist. However, when used as prescribed and monitored, the risk remains low. Still, clinicians watch for signs of misuse or diversion.
Drug Interactions and Precautions
Amphetamine dextroamphetamine interacts with several drugs. Monoamine oxidase inhibitors (MAOIs) can cause dangerous reactions. Avoid MAOIs for at least 14 days before starting.
Other interactions include certain antidepressants and blood pressure medicines. Over-the-counter cold drugs with decongestants also raise heart rate and blood pressure. Always give your clinician a complete medication list.
Medical Conditions That Require Caution
People with heart disease, uncontrolled hypertension, or recent heart attack need careful review. Similarly, a history of substance use disorder requires a balanced approach. Clinicians may suggest alternatives in those cases.
Also, bipolar disorder may worsen if stimulants trigger mania. Doctors often treat mood disorders before or alongside stimulants. Close monitoring reduces risks.
Managing Common Problems
If appetite drops, try high-calorie, nutrient-dense meals at times of higher appetite. Schedule main meals when medication effects are lower, such as evenings. Small, frequent snacks also help maintain nutrition.
For sleep issues, avoid stimulants late in the day. Keep screens off before bed and follow a wind-down routine. If insomnia persists, discuss dose timing or formulation with your clinician.
Handling Missed Doses
If you miss a dose, take it as soon as you remember. However, skip it if it’s close to bedtime. Do not double up to make up a missed dose. Doubling increases side effects and risk.
For XR forms, never crush or chew capsules. Altering formulations can release too much drug at once. Follow administration instructions exactly.
Misuse, Diversion, and Legal Issues
Stimulants carry misuse potential because they boost concentration and alertness. Misuse includes taking higher doses or using others’ prescriptions. Diversion means sharing or selling medication.
Prescribers use strategies to reduce these risks. They may require regular follow-ups, urine drug screens, or pharmacy checks. Educate family members and secure medication at home.
Signs of Misuse
Watch for sudden mood swings, secretive behavior, or lost prescriptions. Rapid weight loss and insomnia can indicate misuse. If you suspect misuse, talk to your clinician urgently.
Disposal matters too. Use take-back programs or follow FDA disposal instructions. Proper disposal keeps medicine out of the wrong hands.
Alternatives and Complementary Treatments
Non-stimulant medications exist, such as atomoxetine and guanfacine. These options work differently and help some people. They may produce fewer stimulant-related side effects.
Behavioral therapy and coaching remain powerful tools. Exercise, sleep, and diet modifications also support symptom control. Consider these as part of a holistic plan.
When to Consider a Switch
Switch if benefits are limited or side effects persist. Also, switch if misuse risk outweighs benefits. Your clinician can guide the transition and tapering schedule.
Switching typically involves gradual changes. Doctors may overlap drugs or pause briefly during the change. Plan carefully to avoid symptom rebound.
Special Populations: Children, Teens, Pregnant People, and Older Adults
Children often respond well to stimulants. Yet caregivers must track growth and mood closely. School cooperation helps manage doses and academic needs.
Teens face unique challenges like peer pressure and driving risks. Parents and clinicians work together on safe storage and education. Moreover, teens learn responsible medication use.
Pregnancy poses risks and benefits to weigh carefully. Stimulants may raise miscarriage risk, though evidence varies. Pregnant people should consult their obstetrician and psychiatrist.
Older adults need lower doses and closer monitoring. They may have heart conditions or take multiple medications. Regular checks reduce complications.
Monitoring and Follow-Up
Routine follow-up is essential. Initially, visits occur every few weeks. Later, clinicians may check every three to six months. Monitoring focuses on symptom control and side effects.
Common monitoring items include weight, blood pressure, and sleep patterns. Behavioral feedback from teachers or family helps assess real-world effects. Labs are rarely required unless other issues arise.
What to Report to Your Clinician
Report mood changes, chest pain, or new tics. Also report severe headaches or unexplained shortness of breath. Mention any new medications, supplements, or substance use.
Keep a symptom diary if possible. Note times of dose, effects, and side effects. That diary helps optimize treatment.
Practical Tips for Parents and Caregivers
Create a consistent daily routine for medication and activities. Label doses and store medication safely. Communicate openly with teachers and therapists.
Encourage healthy eating and adequate sleep. Reward progress and build structure around schoolwork and chores. Finally, maintain regular medical follow-up appointments.
School Strategies
Inform the school nurse about dosing times and side effects. Share the treatment plan with teachers for consistency. Ask for accommodations such as extra time on tests if needed.
Use simple tools like planners and visual schedules. Those tools reinforce medication benefits and improve outcomes.
Cost, Insurance, and Access
Insurance coverage varies by plan and formulation. Generic versions usually cost less. Some manufacturers offer savings programs for branded products.
If cost is a barrier, ask your clinician about generics or prior authorization. Community clinics and patient assistance programs may help provide access.
Pharmacy Tips
Use one pharmacy to fill all controlled substances. That practice prevents duplicate fills. Also, request early refills only when necessary to avoid supply issues.
Keep a copy of your prescription plan and renewals. Controlled substances often need more frequent refills and documentation.
Real-World Tips from Patients
Many patients recommend tracking symptoms daily. Others advise starting at a low dose and increasing slowly. Sharing experiences with support groups can reduce anxiety.
Be honest about side effects and share concerns early. Collaboration with your clinician speeds up the trial-and-error process. Also, combining medication with behavioral changes yields better results.
Safety During Travel and Special Situations
Carry medication in original packaging when flying. Keep copies of your prescription with you. Research local laws about controlled substances if traveling abroad.
If travel crosses time zones, discuss dosing adjustments with your clinician. Avoid abrupt changes without medical advice.
When Treatment Fails to Work
If you don’t respond, your clinician may adjust dose or change drug class. They may also reassess the diagnosis. Co-existing conditions can obscure ADHD symptoms.
Consider a comprehensive re-evaluation. Psychological testing and input from multiple sources often help. Patience and persistence usually lead to better outcomes.
Key Takeaways
Amphetamine dextroamphetamine for ADHD can significantly improve focus and reduce impulsivity. It works by increasing dopamine and norepinephrine. Choosing the right formulation and dose matters a lot.
Combine medication with behavioral strategies for the best results. Monitor side effects and maintain regular follow-up. Finally, communicate openly with your care team and loved ones.
Frequently Asked Questions (FAQs)
1. Can amphetamine dextroamphetamine cure ADHD?
No. It manages symptoms but does not cure ADHD. Long-term coping relies on strategies and supports.
2. Will I become addicted to my medication if I take it as prescribed?
Risk is low with proper medical supervision. However, misuse increases the chance of dependence.
3. Can I drink caffeine while taking amphetamine dextroamphetamine?
Moderate caffeine is usually safe. Yet caffeine can increase jitteriness or insomnia. Monitor how you feel and adjust as needed.
4. How long before I notice an effect?
Most people notice effects within 30 to 60 minutes. Full benefits may require several weeks of monitoring and dose adjustments.
5. Does it affect growth in children?
Some children show slowed growth with long-term stimulant use. Regular monitoring helps detect small changes early.
6. Can I drive while taking this medication?
Yes, most people can drive safely. Remain alert to side effects like dizziness or blurred vision. Don’t drive if you feel impaired.
7. Is it safe during pregnancy or breastfeeding?
Pregnancy and breastfeeding require individualized risk-benefit analysis. Consult obstetric and psychiatric providers before continuing treatment.
8. What should I do if I miss a dose during the day?
Take it when you remember unless it is close to bedtime. Do not double doses to make up for a missed one.
9. How do I store and dispose of my medication?
Store in a locked place away from children. Dispose through take-back programs or follow FDA guidance.
10. Can amphetamine dextroamphetamine worsen anxiety?
It can increase anxiety in some people. If anxiety worsens, discuss alternatives or dose changes with your clinician.
Additional Questions You May Have
1. How will I know the dose is optimal?
Your prescriber will evaluate symptom control and side effects. They may use rating scales and feedback from others. Optimal dose balances benefits and tolerability.
2. Can teenagers manage refills and storage responsibly?
Many teens can learn responsible use. Parents should supervise refills and storage until independence is proven. Consider lockboxes and regular check-ins.
3. Are there objective tests to confirm medication effects?
Clinicians sometimes use cognitive tests or attention measures. However, real-world feedback from school or work often matters most.
4. What happens if my child refuses medication?
Work with the clinician to discuss concerns and alternatives. Behavioral therapies may be an option. Involve the child in decision-making when appropriate.
5. Can I combine amphetamines with non-stimulant ADHD meds?
Sometimes clinicians combine medications. That approach requires careful monitoring and clear rationale. Discuss benefits and risks with your prescriber.
6. Do generics work the same as brand-name drugs?
Generics contain the same active ingredient and generally work similarly. Some people notice minor differences, so monitor effects after switching.
7. How do abrupt stoppages affect me?
Stopping suddenly can lead to fatigue, mood changes, or return of ADHD symptoms. Your clinician may recommend tapering in certain situations.
8. Will insurance cover long-acting versions?
Insurance policies vary. Many plans cover extended-release forms with prior authorization. Ask your provider for assistance.
9. Can exercise replace medication?
Exercise helps symptoms but rarely replaces medication entirely for moderate to severe ADHD. Use exercise as a complementary strategy.
10. What research is emerging about new ADHD treatments?
Researchers study non-stimulant drugs, neuromodulation, and digital therapeutics. Ask your clinician about clinical trials and new options.
References
– National Institute of Mental Health — Attention-Deficit/Hyperactivity Disorder
https://www.nimh.nih.gov/health/topics/attention-deficit-hyperactivity-disorder-adhd
– American Academy of Pediatrics — ADHD: Clinical Practice Guideline for Diagnosis, Evaluation, and Treatment
https://publications.aap.org/pediatrics/article/128/5/1007/71580/Clinical-Practice-Report-ADHD
– U.S. Food and Drug Administration — Adderall (amphetamine and dextroamphetamine) prescribing information
https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/011522s030s031s033s034lbl.pdf
– National Library of Medicine — Amphetamine and Dextroamphetamine: Drug Information
https://medlineplus.gov/druginfo/ (Incomplete: max_output_tokens)