H2: What is Dulaglutide and Why It Matters
Dulaglutide is a once-weekly injectable medication for type 2 diabetes. It belongs to a class called GLP-1 receptor agonists. These medicines help control blood sugar and often support weight loss.
In addition, dulaglutide reduces the risk of some heart problems. Therefore, many clinicians prefer it for people with diabetes and heart disease. This guide focuses on practical tips for safe and effective use.
H2: How Dulaglutide Works
Dulaglutide mimics a natural hormone called GLP-1. As a result, it boosts insulin release when glucose is high. It also slows stomach emptying, which helps control appetite.
Consequently, you will feel fuller longer after meals. Moreover, dulaglutide lowers the liver’s sugar output between meals. This dual action produces steady blood sugar control.
H2: Who Should Use Dulaglutide
Your doctor may recommend dulaglutide if you have type 2 diabetes not controlled by diet and exercise. Doctors often add it when oral medicines fall short. It suits many adults, especially those with heart disease risk.
However, people with type 1 diabetes should not use it. Also, those with a history of certain thyroid cancers should avoid it. Always discuss your medical history with your healthcare team first.
H2: Types of Dulaglutide Products
Several brand options exist, including prefilled pens. Most pens contain a fixed dose and ready-to-use solution. Prefilled pens reduce preparation errors and simplify injections.
A table comparison can help.
H3: Dulaglutide Prefilled Pen Comparison
| Feature | Single-dose pens | Multi-dose pen (if available) |
|—|—:|—:|
| Ready to use | Yes | Varies |
| Dose flexibility | Limited | May offer options |
| Travel friendly | Yes | Depends |
| Storage after opening | Follow label | Follow label |
H2: Dosage and Titration Guidelines
Doctors usually start dulaglutide at a low dose. They raise the dose after a few weeks to reduce side effects. Typical schedules vary, so follow your prescriber’s plan.
Never change the dose without medical advice. If you miss a weekly dose, take it as soon as you remember within 3 days. After that window, skip and take the next dose at the regular time.
H2: Preparing for Injection
Wash your hands with soap and water before handling the pen. Choose a clean, flat surface to set up. Inspect the pen for damage or particles and check the expiration date.
If the pen looks cloudy or discolored, do not use it. Also, let refrigerated pens reach room temperature for 15–30 minutes before injecting. This step reduces injection pain and ensures correct dosing.
H2: Step-by-Step Injection Technique
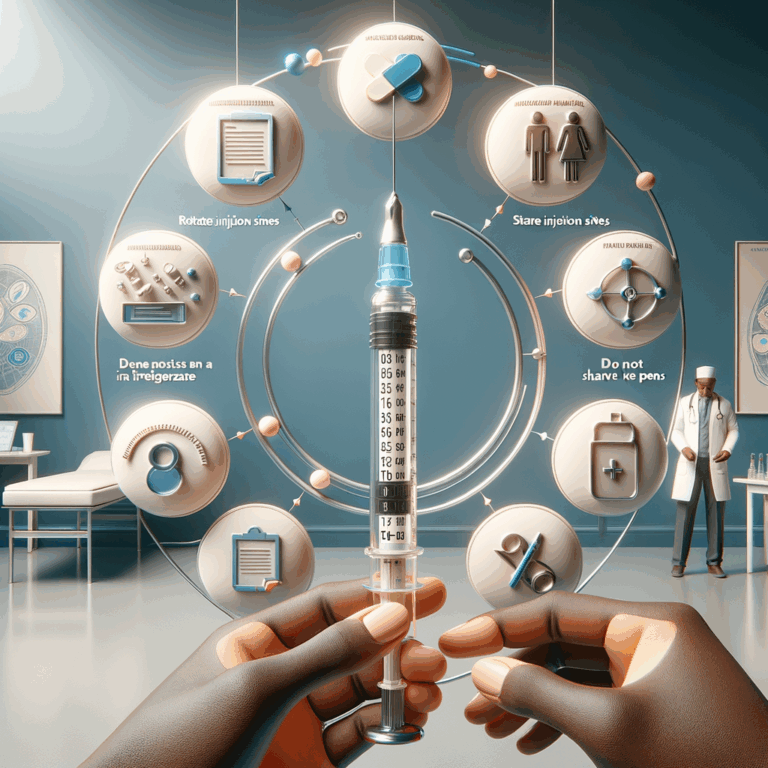
Hold the pen as instructed by the manufacturer. Pinch a fold of skin at the injection site. Insert the needle at a 90-degree angle unless your clinician advises otherwise.
Press the dose button and hold for at least 5–10 seconds to deliver the full dose. Then remove the needle. Dispose of the used pen or needle in a sharps container immediately.
H3: Common Injection Sites
Use these common sites: abdomen, front of thighs, or the back of the upper arms. Rotate sites with each injection to prevent lumps and skin problems. Avoid the same spot for at least one week.
H4: Site Rotation Example
– Week 1: lower abdomen (right)
– Week 2: lower abdomen (left)
– Week 3: front thigh (right)
– Week 4: front thigh (left)
Rotate sources and track sites in a calendar or app.
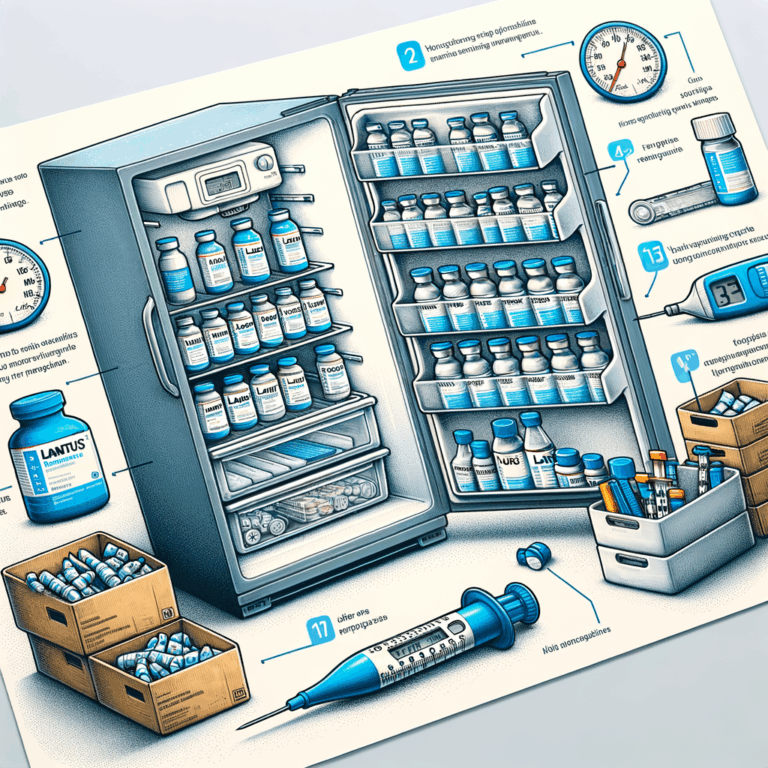
H2: Storage and Handling Tips
Store unopened pens in the refrigerator between 2°C and 8°C (36°F–46°F). Do not freeze them. If a pen freezes, discard it, and use a new one.
Once opened, you may store the pen at room temperature up to the time specified on the label. Keep the cap on to protect from light. Also, avoid storing the pen in direct sunlight or near heat.
H2: Managing Common Side Effects
Nausea, vomiting, and diarrhea are common early on. These symptoms usually lessen over weeks. To ease nausea, eat smaller meals and avoid rich foods.
If you feel dizzy, sit or lie down until you feel better. Severe abdominal pain or persistent vomiting needs urgent medical attention. Call your clinician right away if these occur.
H2: Preventing Injection Site Reactions
Redness, itching, or minor swelling can occur at injection sites. Rotate sites and use proper technique to reduce reactions. Applying a cool compress can relieve discomfort.
If you notice a hard lump or persistent pain, stop using that site. Then contact your healthcare provider. They may evaluate for lipohypertrophy or other issues.
H2: Tips for Staying Consistent with Weekly Doses
Set a fixed day and time for your weekly dose to build a routine. Use phone alarms, calendars, or medication apps for reminders. Pair the injection with a weekly habit, like laundry or trash day.
Also, keep an extra pen at home as backup. Make sure you have refills before your supply runs out. Talk to your pharmacist about automatic refills or delivery programs.
H2: Traveling with Dulaglutide
Pack pens in your carry-on bag, not checked luggage. Bring a doctor’s letter or copy of your prescription to avoid issues with airport security. Keep the pens insulated with a medical cooler or insulated pouch.
If you will be crossing time zones, do not shorten the interval between doses. Instead, take the dose at your usual time in the new zone, or as advised by your clinician. Always carry the manufacturer’s storage instructions.
H2: Injection Safety and Sharps Disposal
Dispose of used pens and needles in an FDA-cleared sharps container. If you don’t have one, use a rigid, puncture-resistant container labeled “Sharps.” Do not throw loose needles in household trash.
When the container fills, follow local rules for disposal. Many pharmacies and health departments offer take-back programs. Never recycle or open the sharps container.
H2: Interactions with Other Diabetes Medications
Dulaglutide often combines well with metformin and SGLT2 inhibitors. It can reduce insulin needs, so monitor glucose closely if you take insulin. Adjustments may be necessary to avoid low blood sugar.
Always tell your clinician about all medicines, supplements, and herbal products. Some drugs can change blood sugar or interact indirectly. Your healthcare team can review your regimen for safety.
H2: Special Populations: Seniors and Children
Clinicians use dulaglutide cautiously in older adults. These patients may face higher risks of dehydration or kidney issues with vomiting. Doctors often start at lower doses and monitor closely.
Dulaglutide is typically not for children with type 1 diabetes. Pediatric use varies by approval status in different regions. Always follow age-specific guidance from pediatric specialists.
H2: Pregnancy and Breastfeeding Considerations
Dulaglutide lacks robust safety data for pregnancy and breastfeeding. Doctors usually stop GLP-1 drugs before conception. If you are pregnant or plan pregnancy, discuss alternatives with your clinician.
If you breastfeed, your provider will weigh benefits and risks. They may switch you to safer options or adjust your diabetes plan. Always consult your healthcare team before changing treatment.
H2: Cost, Insurance, and Financial Assistance
Dulaglutide can cost several hundred dollars per month without insurance. Prices vary by dose and brand. Check with your insurance for coverage and prior authorization needs.
Many manufacturers offer patient assistance, coupons, or copay cards. Nonprofits and local pharmacies may also help. Ask your clinician or pharmacist about programs that reduce out-of-pocket costs.
H2: Monitoring and Follow-Up
Your healthcare team will monitor A1C, weight, and kidney function regularly. They will also review side effects and injection technique. Bring your glucose log to appointments.
Report hypoglycemia, severe nausea, or allergic reactions promptly. If new symptoms appear, your clinician will adjust treatment or order tests. Regular follow-up ensures safety and long-term benefits.
H2: Lifestyle Tips to Maximize Effectiveness
Combine dulaglutide with a balanced diet and regular activity for best results. Small, steady changes in eating and exercise enhance medication effects. Aim for consistent meal timing to reduce glucose spikes.
Stay hydrated and avoid extreme dieting. Rapid weight loss can cause problems. Work with a dietitian or diabetes educator to build a sustainable plan.
H2: When to Contact Your Healthcare Provider
Call your provider for severe stomach pain, prolonged vomiting, or signs of pancreatitis. Also contact them for signs of allergic reaction, like rash or swelling. Any unexplained fainting or breathing trouble needs urgent care.
Seek help if you cannot tolerate the medication or miss multiple doses. Your team can offer alternatives or adjust your regimen. Timely communication prevents complications.
H2: Myths and Misconceptions
Some believe dulaglutide causes immediate, dramatic weight loss. In reality, weight changes appear gradually and vary by person. Medication works best when paired with diet and exercise.
Others worry it destroys the pancreas. While rare pancreatitis associations exist, such events are uncommon. Always report severe abdominal pain so clinicians can evaluate promptly.
H2: Practical Supplies Checklist
– Unopened and opened dulaglutide pens
– Alcohol swabs
– Sharps container
– Needle caps (if separate)
– Insulated travel pouch
– Medication calendar or app
Keep items together in a kit for convenience. Replenish supplies before they run out. This habit reduces missed doses and injection errors.
H2: Frequently Asked Questions (FAQs)
Q1: Can I reuse a dulaglutide pen needle?
A1: No. Use a new needle for each injection. Reusing needles risks infection and dosing errors.
Q2: What if the pen stops working mid-dose?
A2: Stop and contact your provider or pharmacist. Do not try to salvage a partial dose.
Q3: Can I mix dulaglutide with other injectable diabetes drugs at the same site?
A3: Do not inject two medications into the exact same spot consecutively. Space injections and rotate sites.
Q4: How long after the injection does dulaglutide start to work?
A4: It begins to affect blood sugar within hours, but full effects build over weeks.
Q5: Can I drink alcohol while using dulaglutide?
A5: Moderate alcohol can be okay, but it may worsen nausea or affect blood sugar. Discuss limits with your clinician.
Q6: Will dulaglutide affect my vaccines or other injections?
A6: It usually does not affect vaccines. However, space injections if unsure and ask your provider.
Q7: What if I develop severe nausea?
A7: Contact your clinician. They may lower dose, slow titration, or suggest anti-nausea measures.
Q8: Is weight loss guaranteed with dulaglutide?
A8: No. Many people lose weight, but results vary. Lifestyle changes enhance the effect.
Q9: How do I dispose of a partially used pen?
A9: If the pen is designed for single use, dispose of it. Follow manufacturer instructions.
Q10: Can I stop dulaglutide suddenly?
A10: You can stop, but consult your provider first. Stopping may raise blood sugar, needing other treatments.
H2: Final Practical Tips and Takeaways
Keep a routine and use reminders to avoid missed weekly doses. Store pens properly and check expiration dates. Rotate injection sites and track reactions.
Speak openly with your healthcare team about side effects, costs, and technique. With careful use, dulaglutide can offer meaningful benefits for many people living with type 2 diabetes.
H2: Additional FAQs (Reader Questions Not Fully Covered Above)
Q1: How does dulaglutide compare with other weekly GLP-1s?
A1: Differences include molecular structure, dosing, side effect profiles, and cost. Your clinician can compare based on your needs.
Q2: Are there long-term safety concerns beyond five years?
A2: Long-term data is still growing. Continue routine monitoring and discuss new findings with your provider.
Q3: Can I take dulaglutide if I have a history of pancreatitis years ago?
A3: Clinicians usually exercise caution. They will weigh risks and monitor closely if they prescribe it.
Q4: Does dulaglutide affect blood pressure or cholesterol?
A4: Indirectly. Weight loss and improved glucose control can improve these numbers. However, direct effects vary.
Q5: Will dulaglutide require periodic lab tests beyond A1C?
A5: Yes. Kidney function tests and other labs may be needed depending on your health.
Q6: Can dulaglutide cause depression or mood changes?
A6: Mood changes are uncommon, but report any new psychiatric symptoms immediately to your provider.
Q7: What alternatives exist if I cannot tolerate dulaglutide?
A7: Alternatives include other GLP-1 agents, DPP-4 inhibitors, SGLT2 inhibitors, or insulin therapy. Your clinician can advise.
Q8: Can I use dulaglutide for weight loss alone?
A8: Off-label use varies by region. Some GLP-1s have weight-loss approvals. Only use as prescribed by a clinician.
Q9: Does dulaglutide affect exercise performance?
A9: It generally does not harm exercise ability. If you feel dizzy or weak, stop and reassess your plan.
Q10: How do I transition from daily GLP-1 injections to weekly dulaglutide?
A10: Your clinician will design a transition plan. They consider last dose timing and allow overlap if needed.
H2: References
– Eli Lilly and Company. Trulicity (dulaglutide) Prescribing Information. https://uspl.lilly.com/trulicity/trulicity.html
– American Diabetes Association. Standards of Care in Diabetes. https://diabetes.org/diabetes/medication-management
– FDA. Trulicity Drug Safety Communication. https://www.fda.gov/drugs/drug-safety-and-availability
– National Institute for Health and Care Excellence (NICE). GLP-1 receptor agonists guidance. https://www.nice.org.uk/guidance
Note: This guide provides general information and does not replace professional medical advice. Always follow your healthcare provider’s instructions.