- Understanding Gabapentin for Nerve Pain
- How Gabapentin Works: The Basics
- Conditions Commonly Treated with Gabapentin
- Starting Gabapentin: What to Expect
- Typical Dosing Strategies
- Maximizing Relief: Practical Tips
- Medication Timing and Consistency
- What to Do If You Miss a Dose
- Reducing Side Effects
- Managing Common Side Effects
- Interactions and Safety Considerations
- Drugs That May Interact with Gabapentin
- When Gabapentin Might Not Work
- Alternative Therapies to Consider
- Tapering and Stopping Gabapentin Safely
- Signs You Might Need to Stop or Adjust Treatment
- Special Populations: What to Know
- Kidney Disease and Dose Adjustments
- Practical Daily Tips to Boost Relief
- Combining Gabapentin with Exercise
- Lifestyle Changes That Complement Medication
- Sleep Hygiene for Pain Relief
- Cost, Access, and Generic Options
- Formulations: Which One to Choose?
- Monitoring Progress: What to Track
- When to Call Your Doctor
- Real-Life Tips from Patients
- Common Myths and Misconceptions
- Emerging Research and Future Directions
- Questions Researchers Are Asking
- Summary: Key Takeaways
- FAQs
- References
Understanding Gabapentin for Nerve Pain
Gabapentin for nerve pain has become a go-to option for many people. Doctors often prescribe it for neuropathic pain, especially when other treatments fail. Consequently, more patients ask about how it works, what to expect, and how to get the best relief.
In plain terms, gabapentin affects the way nerves send pain signals to your brain. It doesn’t cure the underlying nerve damage. However, it can reduce burning, shooting, or tingling sensations. Most importantly, it can restore function and improve sleep for many people.
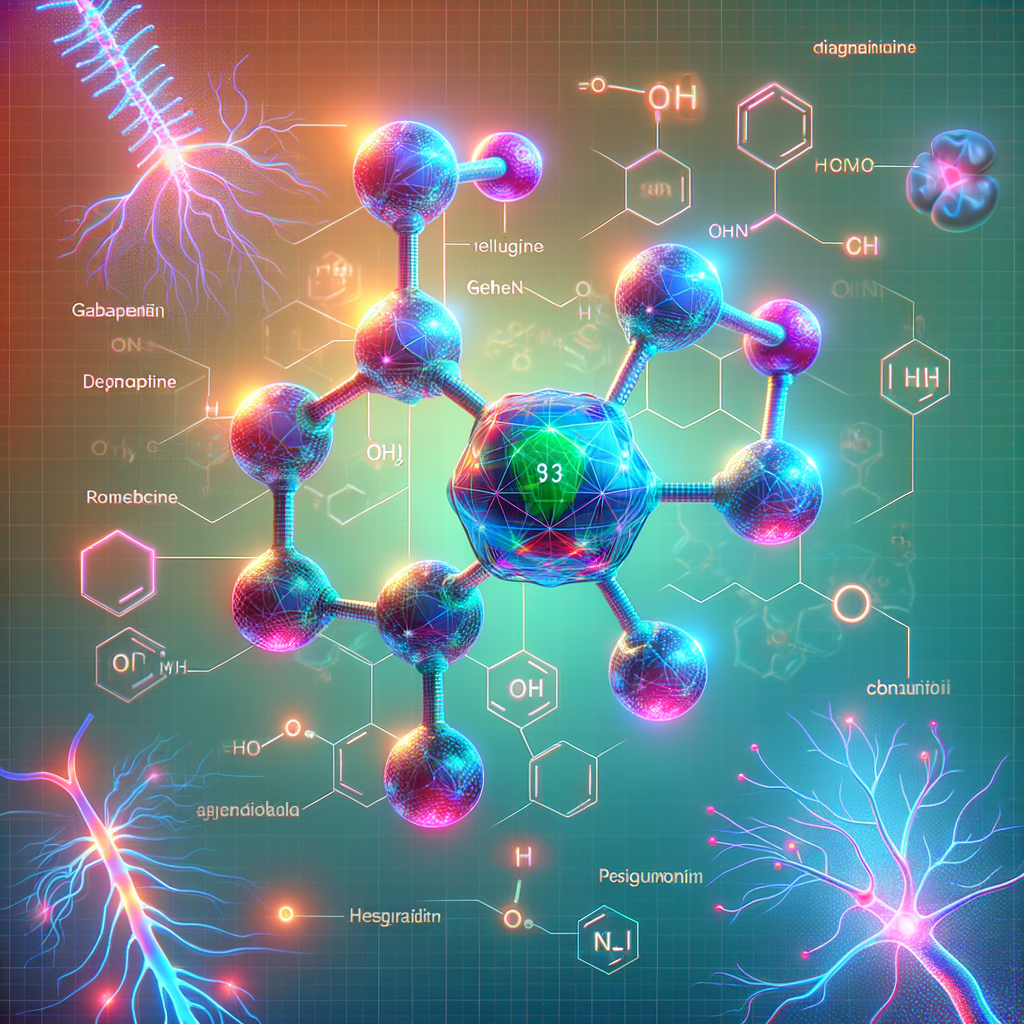
How Gabapentin Works: The Basics
Gabapentin mimics a naturally occurring neurotransmitter in the brain. It binds to calcium channels on nerve cells. As a result, it reduces abnormal electrical activity that causes pain.
Therefore, gabapentin can calm overactive nerves. However, the exact mechanism still puzzles researchers. They agree it affects signal release, and thus pain perception, in multiple ways.
Conditions Commonly Treated with Gabapentin
Gabapentin helps with diabetic neuropathy, postherpetic neuralgia, and certain nerve injuries. Also, physicians sometimes use it for fibromyalgia or chronic pain syndromes. Off-label uses include anxiety and migraine prevention.
Each condition responds differently. Hence, doctors tailor the dose to your symptoms and medical history. Always follow medical advice and report side effects promptly.
Starting Gabapentin: What to Expect
When you start gabapentin, doctors usually recommend a low dose. They then increase the dose slowly over days or weeks. This approach helps reduce side effects like dizziness or drowsiness.
Most patients notice some improvement within one to two weeks. However, full relief may take several weeks. If you see no improvement after a month, discuss alternatives with your provider.
Typical Dosing Strategies
Dosing varies by condition and response. For neuropathic pain, a common starting dose is 300 mg at night. Clinicians then increase it to 300 mg two or three times daily. Some patients need up to 2,400 mg per day for adequate control.
Below is a simple dosing table that shows common titration patterns.
| Week | Common Dose | Notes |
|---|---|---|
| Week 1 | 300 mg at night | Start low to reduce side effects |
| Week 2 | 300 mg twice daily | Assess tolerance |
| Week 3 | 300 mg three times daily | Evaluate effectiveness |
| Weeks 4+ | Adjust to 900–2400 mg/day | Customize based on relief and side effects |
Maximizing Relief: Practical Tips
Combine gabapentin with lifestyle changes for better results. Regular exercise, stretching, and weight management reduce nerve stress. Additionally, improving sleep boosts pain tolerance.
Use heat or cold therapy when appropriate. For example, apply a warm pack to stiff muscles. Conversely, use a cold pack for acute swelling or sharp pain. Together, these measures support medication effects.
Medication Timing and Consistency
Take gabapentin at the same times every day. This practice keeps blood levels steady. As a result, you reduce breakthrough pain.
If your doctor prescribes multiple doses, space them evenly. For instance, take doses morning, afternoon, and night. Also, avoid missing doses to maintain relief.
What to Do If You Miss a Dose
If you miss a dose, take it as soon as you remember. However, skip it if the next dose is near. Never double up to catch up. Doubling can increase side effects.
Instead, call your provider if you frequently miss doses. They can suggest a schedule that fits your routine.
Reducing Side Effects
Gabapentin can cause dizziness, drowsiness, and unsteadiness. Fortunately, most side effects lessen over time. Start at lower doses and increase slowly to lower risk.
Avoid alcohol and sedatives while on gabapentin. Combining them increases drowsiness and breathing issues. Also, be cautious with activities that require alertness, like driving, until you know how gabapentin affects you.
Managing Common Side Effects
To ease dizziness, stand up slowly from sitting or lying positions. If you feel sleepy, consider taking your largest dose at night. If nausea occurs, take gabapentin with food.
If side effects persist or worsen, contact your healthcare provider. They may adjust your dose, change timing, or switch medications.
Interactions and Safety Considerations
Gabapentin interacts with certain medications and conditions. For example, antacids containing aluminum or magnesium can reduce gabapentin absorption. Take gabapentin at least two hours after such antacids.
People with kidney problems need dose adjustments. Your provider will calculate the right dose based on kidney function. Also, women who are pregnant or breastfeeding should discuss risks and benefits with their doctor.
Drugs That May Interact with Gabapentin
– Opioids and benzodiazepines can increase sedation and respiratory depression.
– Antacids reduce gabapentin absorption.
– Some sleep medicines and muscle relaxants increase drowsiness.
Always tell your provider about all prescription and over-the-counter drugs. Include supplements and herbal products.
When Gabapentin Might Not Work
Not everyone gains enough relief from gabapentin. Some types of nerve pain respond poorly. For instance, pain caused by ongoing mechanical compression may need surgery or targeted therapy.
If gabapentin fails, doctors may try pregabalin, duloxetine, or tricyclic antidepressants. Sometimes, combining drugs yields better outcomes. Discuss options based on your pain type and health profile.
Alternative Therapies to Consider
In addition to medications, consider nerve blocks, physical therapy, and transcutaneous electrical nerve stimulation (TENS). Cognitive behavioral therapy can also help you cope with chronic pain.
For certain conditions, topical agents like lidocaine or capsaicin offer relief. Each option has trade-offs. Therefore, choose treatments with your clinician.
Tapering and Stopping Gabapentin Safely
Never stop gabapentin abruptly. Doing so can cause withdrawal symptoms like anxiety, insomnia, and sweating. Also, some people experience increased pain or seizures.
Your doctor will create a tapering schedule. Typically, they reduce the dose gradually over weeks. Follow their instructions and report any withdrawal symptoms.
Signs You Might Need to Stop or Adjust Treatment
Seek immediate help for severe side effects like breathing trouble or extreme drowsiness. Also, report allergic reactions or swelling. If pain worsens or new symptoms arise, consult your provider.
Your provider may adjust the dose or switch drugs. They may also order tests to check kidney function or other causes of symptoms.
Special Populations: What to Know
Older adults often develop more side effects from gabapentin. They also face higher fall risk. Therefore, doctors usually start at lower doses and increase slowly for seniors.
Children and pregnant women require special considerations. Pediatric uses differ, and safety in pregnancy depends on the situation. Always discuss risks and benefits with a specialist.
Kidney Disease and Dose Adjustments
Kidney function affects gabapentin clearance. Lower kidney function means gabapentin stays in the body longer. Consequently, doctors reduce doses to avoid toxicity.
If you have kidney disease, bring recent lab results to your appointment. That information helps your provider choose a safe dose.
Practical Daily Tips to Boost Relief
Small daily habits improve the effectiveness of gabapentin. For instance, set alarms to keep a consistent schedule. Use pill organizers to avoid missed doses.
Also, keep a pain diary. Note dose times, pain levels, and triggers. Bring this diary to appointments. It helps your doctor tailor your plan.
Combining Gabapentin with Exercise
Gentle exercise benefits nerve health and reduces pain intensity. Walk, swim, or do low-impact aerobics several times per week. Stretch daily to keep nerves mobile.
Start slowly and increase activity gradually. If exercise increases pain, scale back and consult a physical therapist.
Lifestyle Changes That Complement Medication
Quit smoking to improve circulation and nerve healing. Maintain a healthy weight to reduce pressure on nerves. Control blood sugar if you have diabetes.
Also, manage stress through relaxation techniques. Meditation, deep breathing, or guided imagery can lower pain perception. These skills improve outcomes with gabapentin.
Sleep Hygiene for Pain Relief
Poor sleep worsens pain. Stick to a consistent sleep schedule every day. Avoid screens before bedtime and create a quiet sleep environment.
Consider cognitive behavioral therapy for insomnia (CBT-I) if sleep problems persist. Better sleep often means less pain.
Cost, Access, and Generic Options
Gabapentin comes in generic forms, which are affordable. Many insurance plans cover it for neuropathic pain. Your pharmacist can suggest the most cost-effective option.
Patient assistance programs and coupons sometimes lower costs further. Ask your provider or pharmacist about available options. They can guide you to savings.
Formulations: Which One to Choose?
Gabapentin comes as immediate-release, extended-release, and oral solution. Immediate-release requires multiple daily doses. Extended-release often allows once-daily dosing.
Your doctor will choose a formulation based on your needs. For instance, if night pain troubles you, an evening extended-release dose may help.
Monitoring Progress: What to Track
Track pain intensity, sleep quality, mood, and daily function. Use a numeric pain scale or a diary app. These records help your doctor fine-tune treatment.
Also, monitor side effects like dizziness and weight changes. Periodic lab tests may assess kidney function. Keep your healthcare team informed.
When to Call Your Doctor
Contact your provider for new or worsening symptoms. Also, seek help for severe side effects, falls, or breathing problems. If pain becomes intolerable, ask about alternative treatments.
Your provider may need to change dosing or try other therapies. Timely communication prevents complications.
Real-Life Tips from Patients
Many patients find slow titration helps them tolerate gabapentin. Others report that taking the largest dose at night reduces daytime drowsiness. Some use pill organisers and timers to stay consistent.
People also combine gabapentin with physical therapy and relaxation techniques. These multi-pronged strategies often yield better results than medication alone.
Common Myths and Misconceptions
Myth: Gabapentin is addictive like opioids. Fact: Gabapentin has a lower abuse potential than opioids. However, some people misuse it. Therefore, follow medical guidance.
Myth: Gabapentin cures nerve damage. Fact: It manages symptoms but does not reverse nerve injury. Treat the root cause when possible.
Emerging Research and Future Directions
Researchers continue to study gabapentin’s role in pain management. New studies explore combination therapies and long-term effects. Also, scientists examine biomarkers to predict who will respond.
Future options may include personalized dosing based on genetics. For now, clinicians rely on symptom monitoring and patient feedback.
Questions Researchers Are Asking
– Which patient subgroups benefit most from gabapentin?
– What long-term side effects appear with prolonged use?
– How can clinicians minimize misuse while preserving access for patients in need?
These questions will shape future guidelines and practices.
Summary: Key Takeaways
Gabapentin for nerve pain offers meaningful relief for many people. Start low, go slow, and follow your doctor’s plan. Combine medication with lifestyle changes, exercise, and good sleep.
Monitor side effects and kidney function. Avoid alcohol and sedatives. Communicate regularly with your healthcare team to optimize outcomes.
FAQs
1. Can gabapentin completely eliminate nerve pain?
Gabapentin can significantly reduce pain for many people. However, it rarely eliminates nerve pain entirely. It works best when combined with other treatments and lifestyle changes.
2. How long does gabapentin take to work for nerve pain?
Some people notice improvement in one to two weeks. However, it can take several weeks for full benefit. Your provider may adjust the dose during that period.
3. Is gabapentin addictive?
Gabapentin has a lower addiction potential than opioids. Still, misuse and dependence can occur, especially with high doses or combined sedatives. Use gabapentin only as prescribed.
4. Can I drink alcohol while taking gabapentin?
Avoid alcohol. Alcohol increases drowsiness and breathing problems. Also, combining alcohol with gabapentin raises fall risk.
5. What should I do if gabapentin causes severe drowsiness?
Tell your doctor right away. They may lower your dose or change the dosing schedule. Taking your largest dose at night sometimes helps.
6. Can gabapentin cause weight gain?
Some patients report modest weight gain. Changes in appetite or activity may contribute. Discuss weight concerns with your provider.
7. Is gabapentin safe during pregnancy?
Gabapentin may pose risks during pregnancy. Your doctor will weigh benefits and risks. Do not stop gabapentin abruptly if you’re pregnant.
8. Can gabapentin interact with my antacid?
Yes. Antacids containing aluminum or magnesium can reduce gabapentin absorption. Take gabapentin at least two hours after such antacids.
9. What happens if I stop gabapentin suddenly?
Stopping suddenly can trigger withdrawal symptoms like anxiety, insomnia, and sweats. Your doctor will guide a gradual taper.
10. How do I know if gabapentin is the right choice for my nerve pain?
Your doctor will evaluate your pain type, medical history, and kidney function. If first-line therapies fail or aren’t suitable, gabapentin may be a good option.
References
– National Center for Biotechnology Information — Gabapentin. https://www.ncbi.nlm.nih.gov/books/NBK548161/
– U.S. Food & Drug Administration — Gabapentin Drug Safety Communication. https://www.fda.gov/drugs/postmarket-drug-safety-information-patients-and-providers/gabapentin-information
– American Academy of Neurology — Guidelines on Neuropathic Pain. https://www.aan.com/Guidelines/home/GuidelineDetail/164
– Mayo Clinic — Gabapentin (Oral Route). https://www.mayoclinic.org/drugs-supplements/gabapentin-oral-route/description/drg-20064011
– Johns Hopkins Medicine — Neuropathic Pain: Diagnosis and Treatment. https://www.hopkinsmedicine.org/health/conditions-and-diseases/neuropathic-pain
If you’d like, I can create a printable pain diary template. Also, I can draft a sample tapering plan you can bring to your provider. Which would help you most?