- Introduction
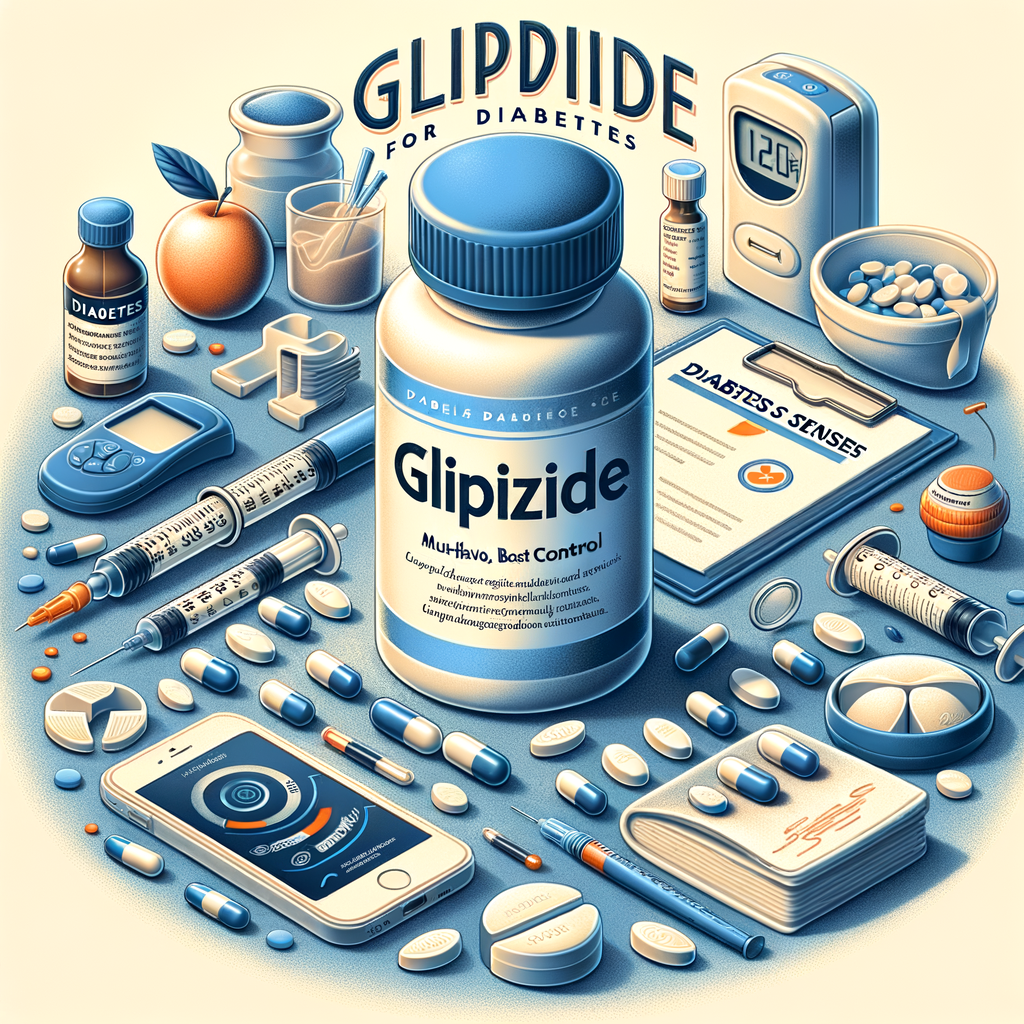
- What Is Glipizide?
- Key Features of Glipizide
- How Glipizide Works
- Mechanism in Simple Terms
- Who Should Use Glipizide?
- Ideal Candidates
- Forms and Dosing
- Typical Dosing Table
- Dosing Tips
- Effectiveness and Benefits
- Benefits at a Glance
- Potential Side Effects
- Managing Side Effects
- Drug Interactions and Precautions
- Common Interacting Drugs
- Monitoring While on Glipizide
- What to Track at Home
- Special Populations
- Kidney and Liver Considerations
- Combining Glipizide with Other Diabetes Medicines
- Common Combination Strategies
- Lifestyle Strategies to Enhance Control
- Practical Lifestyle Tips
- Troubleshooting Common Issues
- When to Call Your Doctor
- Comparing Glipizide with Other Treatments
- Pros and Cons Summary
- Practical Tips for Everyday Use
- Daily Checklist
- Cost and Accessibility
- Saving Strategies
- Long-Term Outlook with Glipizide
- Maintaining Control Over Time
- Patient Stories and Real-World Use
- Common Patient Experiences
- Conclusion
- Frequently Asked Questions
- 1. Can glipizide cure diabetes?
- 2. How quickly does glipizide start working?
- 3. Is glipizide safe for older adults?
- 4. Can I drink alcohol while on glipizide?
- 5. Is glipizide used for type 1 diabetes?
- 6. What should I do if I miss a dose?
- 7. Can glipizide cause weight gain?
- 8. How does glipizide compare with metformin?
- 9. Will I need to stop glipizide before surgery?
- 10. How do I treat a severe hypoglycemia episode?
- References
Introduction
Glipizide for Diabetes has helped millions manage blood sugar. Most people know about insulin. Yet many adults with type 2 diabetes start with oral medicines. Glipizide stands out for its effectiveness and affordability. In this article, I explain how it works. I also show how to use it safely. Finally, I offer practical tips for best control.
This guide keeps things clear and actionable. Each section uses short sentences. Moreover, I use a friendly, conversational tone. Therefore, you can learn without getting bogged down in jargon. Let’s begin.
What Is Glipizide?
Glipizide belongs to the sulfonylurea class of drugs. Doctors prescribe it for type 2 diabetes. It helps lower blood glucose by stimulating insulin release. Patients usually take it by mouth once or twice daily.
This medicine dates back to the 1970s. Since then, many users have relied on it for steady glucose control. While newer drugs exist, glipizide remains a mainstay. It balances effectiveness with cost.
Key Features of Glipizide
– Stimulates insulin secretion from pancreatic beta cells.
– Works best when some insulin production remains.
– Available in immediate-release and extended-release.
– Generally taken before meals or as prescribed.
These features make Glipizide for Diabetes a practical option for many people. However, it requires monitoring. You must watch for side effects like hypoglycemia. With the right care, it helps maintain healthy glucose ranges.
How Glipizide Works
Glipizide binds to potassium channels on beta cells. This action closes the channels. Consequently, calcium flows into the cells. That triggers insulin release. More insulin lowers blood glucose.
Importantly, glipizide acts only when beta cells respond. Thus, people with minimal insulin production get less benefit. In contrast, those with residual insulin secretion often see good results. The drug complements diet and exercise. Together, they reduce elevated glucose.
Mechanism in Simple Terms
– Glipizide targets beta cells in the pancreas.
– It stimulates insulin release when glucose rises.
– The extra insulin helps cells take up sugar.
– As a result, blood glucose decreases.
This mechanism explains why timing and dosing matter. Taking glipizide without food can raise the risk of low blood sugar. That risk changes how doctors advise dosing.
Who Should Use Glipizide?
Doctors prescribe Glipizide for Diabetes mainly for adults with type 2 diabetes. They choose it when lifestyle changes alone do not control glucose. Often, clinicians add it when metformin is insufficient. Patients who cannot tolerate metformin may start glipizide.
However, not everyone qualifies. People with type 1 diabetes should not use it. Also, people without enough pancreatic insulin production may not respond. Doctors evaluate medical history, kidney function, and other medications.
Ideal Candidates
– Adults with type 2 diabetes and residual insulin production.
– Patients needing a low-cost oral agent.
– People who take medications with a low interaction risk.
– Those who can monitor blood sugar regularly.
Conversely, doctors avoid glipizide for patients prone to severe hypoglycemia. They also avoid it in those with certain liver or kidney issues. A careful medical review ensures safe use.
Forms and Dosing
Glipizide comes as immediate-release tablets and extended-release tablets. Immediate-release usually requires split doses. Extended-release provides steady levels with once-daily dosing. Always follow your prescriber’s instructions.
Below is a simple dosing guide. Note that doctors adjust doses based on response and side effects. Never change your dose without medical advice.
Typical Dosing Table
| Form | Starting Dose | Usual Range | Max Dose |
|---|---|---|---|
| Immediate-release | 2.5–5 mg once or twice daily | 2.5–20 mg per day | 40 mg/day |
| Extended-release | 5 mg once daily | 5–20 mg once daily | 20 mg/day |
Keep the tablet whole if it’s extended-release. Crushing can release too much drug at once. That increases hypoglycemia risk.
Dosing Tips
Take immediate-release tablets 30 minutes before a meal. That timing helps prevent low blood sugar. Take extended-release tablets with breakfast. Also, maintain consistent meal patterns. Consistency improves glucose control.
If you miss a dose, take it as soon as you remember. Skip it if it’s nearly time for your next dose. Do not double up on doses in one day.
Effectiveness and Benefits
Studies show glipizide lowers HbA1c by about 1 to 2 percentage points. That result compares well with many other oral medicines. Moreover, it works quickly within days to weeks. Many people notice lower fasting glucose within a week.
Beyond glucose lowering, glipizide often improves quality of life. Taking an oral pill feels simpler than injections for many people. Also, the drug is widely available and affordable. This accessibility matters in long-term diabetes care.
Benefits at a Glance
– Rapid glucose lowering.
– Effective HbA1c reduction.
– Oral dosing increases convenience.
– Cost-effective compared to newer agents.
Despite its strengths, glipizide does not address insulin resistance directly. Therefore, combining it with lifestyle changes and other medicines often yields better outcomes.
Potential Side Effects
Like all medicines, glipizide causes side effects in some people. The most serious risk is hypoglycemia. Symptoms include sweating, dizziness, shaking, and confusion. Severe hypoglycemia can cause fainting or seizures.
Other common side effects include weight gain, nausea, and skin rash. Rarely, it may cause liver problems or blood disorders. If you notice signs like jaundice or unusual bruising, seek medical help immediately.
Managing Side Effects
– Monitor blood sugar closely, especially at first.
– Carry a quick sugar source like glucose tablets.
– Eat regular meals to reduce hypoglycemia risk.
– Report any unusual symptoms to your doctor.
If hypoglycemia happens often, your provider may lower the dose. Alternatively, they may change your medicine.
Drug Interactions and Precautions
Glipizide interacts with several drugs. Some medications raise the risk of low blood sugar. Others reduce glipizide’s effectiveness. For example, certain antibiotics and heart medicines can affect blood sugar control.
Additionally, alcohol can increase the risk of low blood sugar. It can also cause flushing when combined with glipizide. Meanwhile, corticosteroids and some thyroid medicines can raise blood glucose. These interactions may require dose adjustments.
Common Interacting Drugs
– Beta-blockers: may mask hypoglycemia symptoms.
– Warfarin: may alter clotting control.
– Certain antibiotics: can increase hypoglycemia risk.
– Antifungals like fluconazole: may change blood levels.
Always tell your prescriber about all prescriptions and supplements. Your pharmacist can also check for interactions.
Monitoring While on Glipizide
Monitoring helps you use Glipizide for Diabetes safely. Check fasting blood glucose regularly. Also, measure glucose before activities that raise hypoglycemia risk. Your provider will order HbA1c tests every 3 months or as needed.
Periodically, doctors check liver and kidney function. These tests ensure proper dosing and detect problems early. Report any signs of low blood sugar immediately. Prompt action prevents complications.
What to Track at Home
– Fasting and pre-meal blood glucose.
– Symptoms of hypoglycemia and hyperglycemia.
– Weight and diet changes.
– Any side effects like rashes or weakness.
Use a log or app to record readings. Share this information with your healthcare team. It helps them tailor your treatment.
Special Populations
Certain groups need extra caution with glipizide. Elderly individuals often face higher hypoglycemia risk. Therefore, clinicians start them on lower doses. They also monitor them more closely.
Pregnancy and breastfeeding pose concerns. Doctors prefer insulin during pregnancy. They avoid glipizide if a safer alternative exists. Meanwhile, children rarely use this medicine.
Kidney and Liver Considerations
Reduced kidney or liver function changes how glipizide behaves. The drug’s breakdown slows in liver disease. That increases the risk of prolonged low blood sugar. Likewise, severe kidney disease may cause drug accumulation.
Therefore, providers adjust doses based on labs. They may choose another medicine if risks outweigh benefits.
Combining Glipizide with Other Diabetes Medicines
Doctors often combine glipizide with metformin. This pairing improves both insulin secretion and insulin sensitivity. Other combinations include glipizide with DPP-4 inhibitors or insulin.
When combining medicines, the hypoglycemia risk often increases. Therefore, careful monitoring and dose adjustments matter. Your provider will design a plan that balances benefits and risks.
Common Combination Strategies
– Glipizide + Metformin: widely used, effective.
– Glipizide + DPP-4 inhibitor: lower hypoglycemia risk.
– Glipizide + Insulin: used in specific cases with caution.
Always follow your provider’s recommendations. Never add other diabetes drugs on your own.
Lifestyle Strategies to Enhance Control
Glipizide for Diabetes works best with healthy habits. Regular physical activity helps lower glucose and improves insulin sensitivity. Likewise, a balanced diet stabilizes blood sugar.
Eating consistent meals reduces hypoglycemia episodes. Focus on whole foods that contain fiber and lean protein. Avoid sugary drinks and large, high-carb meals.
Practical Lifestyle Tips
– Walk for 30 minutes most days.
– Include vegetables, whole grains, and lean protein.
– Eat consistent portions and meal times.
– Limit alcohol and sugary beverages.
– Stop smoking to reduce cardiovascular risk.
By combining medication and lifestyle changes, you get the best outcomes.
Troubleshooting Common Issues
If you experience frequent low blood sugar, don’t panic. First, check meal timing and portions. You may need a dose adjustment. Also, consider drug interactions if you recently started another medicine.
If your glucose stays high, review medication adherence. Also, reassess diet and activity levels. Your provider may increase the dose or add a second medication. Regular communication prevents long-term complications.
When to Call Your Doctor
– Repeated hypoglycemia or severe symptoms.
– Symptoms like jaundice or severe fatigue.
– Unexpected weight loss or persistent high glucose.
– Side effects that affect daily life.
Early contact helps avoid emergencies and keeps your treatment on track.
Comparing Glipizide with Other Treatments
Compared to metformin, glipizide lowers glucose but does not improve insulin sensitivity. However, glipizide often works faster. Newer agents like SGLT2 inhibitors and GLP-1 receptor agonists offer additional benefits. These benefits include weight loss and heart protection.
Yet, newer agents come at a higher cost. In many settings, glipizide remains a cost-effective option. The choice depends on individual priorities and medical status.
Pros and Cons Summary
Pros:
– Effective glucose lowering.
– Oral dosing convenience.
– Lower cost than many newer drugs.
Cons:
– Higher hypoglycemia risk.
– Potential weight gain.
– Limited cardiovascular and renal benefits compared to others.
Talk with your provider about your priorities. They can guide the best choice for you.
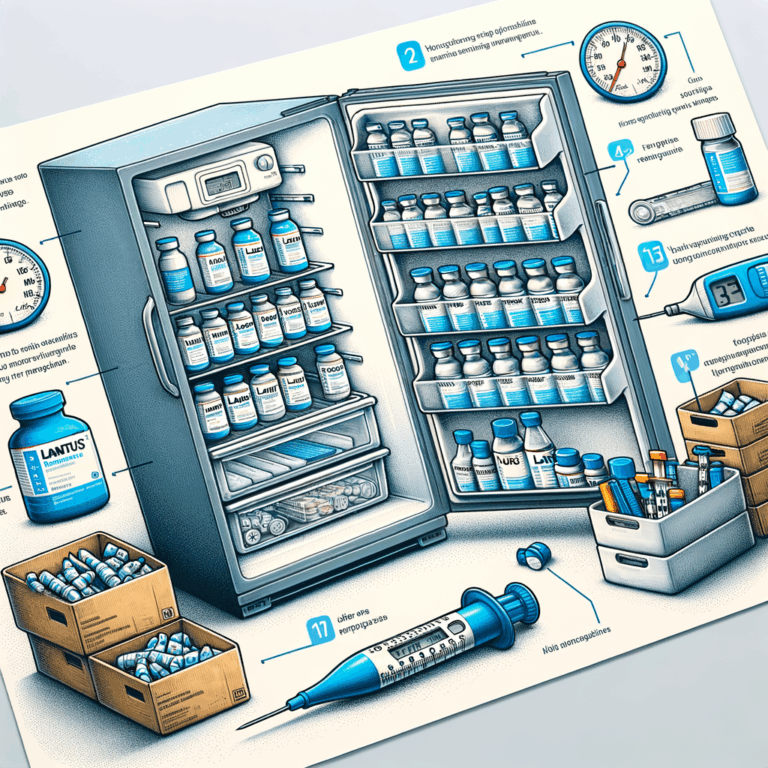
Practical Tips for Everyday Use
Store glipizide at room temperature away from moisture. Take tablets consistently with meals. Keep an emergency sugar source handy at all times. Also, wear medical ID if you are at risk for severe hypoglycemia.
If you travel, pack extra medication and a copy of your prescription. Check time zones when scheduling doses. Finally, always dispose of expired medication safely.
Daily Checklist
– Take medication as prescribed.
– Test blood glucose according to plan.
– Carry glucose tablets or snacks.
– Note any new symptoms or side effects.
– Keep a list of current medications.
This simple routine reduces surprises and promotes steady control.
Cost and Accessibility
Glipizide ranks among the more affordable diabetes medications. Generic versions further lower cost. Insurance plans often cover it under tiered formularies. This accessibility makes it a practical choice globally.
Nevertheless, price can vary by region and pharmacy. Many patient assistance programs help with costs. Ask your pharmacist or provider if you need financial support.
Saving Strategies
– Use generic glipizide when possible.
– Compare pharmacy prices or use discount cards.
– Check manufacturer assistance programs.
– Buy a longer supply if savings apply.
Staying within budget improves adherence. Better adherence leads to better glucose control.
Long-Term Outlook with Glipizide
Many people use glipizide successfully for years. However, diabetes is progressive for some. Over time, beta cell function may decline. If that happens, glipizide may become less effective.
In such cases, your provider may switch to or add other medicines. They may also consider insulin therapy. Regular follow-up ensures treatment evolves with your needs.
Maintaining Control Over Time
– Keep regular healthcare appointments.
– Monitor HbA1c and other labs as recommended.
– Update your care plan when life changes occur.
– Maintain healthy lifestyle habits.
Consistent care preserves health and reduces complications over the long term.
Patient Stories and Real-World Use
Many patients report fast improvements in fasting glucose with glipizide. They often appreciate the ease of a daily pill. Some users do encounter hypoglycemia early on. Yet, with education and monitoring, they manage it well.
Doctors highlight glipizide’s value in resource-limited settings. It offers a reliable option when cost matters. Still, clinicians tailor therapy to each person’s needs and risks.
Common Patient Experiences
– Early glucose improvement within weeks.
– Need for lifestyle adjustments to avoid lows.
– Occasional dose tweaks to find the right balance.
– Long-term use until beta cell decline requires change.
These real-world outcomes show the practical role of Glipizide for Diabetes.
Conclusion
Glipizide for Diabetes offers a proven, affordable way to lower blood glucose. It works by boosting insulin release. With proper monitoring, it provides meaningful HbA1c reductions. Yet, it carries a higher hypoglycemia risk than some newer agents.
To get the best control, combine glipizide with lifestyle changes. Also, keep regular follow-ups and lab checks. If problems arise, your healthcare team can adjust therapy. In short, glipizide remains a valuable tool when used carefully.
Frequently Asked Questions
1. Can glipizide cure diabetes?
No. Glipizide controls blood glucose but does not cure diabetes. It helps manage symptoms and reduce complications risk.
2. How quickly does glipizide start working?
You often see lower fasting glucose within days to a week. Full HbA1c changes take about 2 to 3 months.
3. Is glipizide safe for older adults?
It can be safe with caution. Doctors start older adults on lower doses. They monitor for hypoglycemia closely.
4. Can I drink alcohol while on glipizide?
Alcohol increases hypoglycemia and may cause flushing. Limit alcohol and discuss risks with your doctor.
5. Is glipizide used for type 1 diabetes?
No. Glipizide requires some insulin production. Type 1 diabetes lacks this, so insulin therapy is needed.
6. What should I do if I miss a dose?
Take it as soon as you remember unless it’s near the next dose. Do not double your dose to catch up.
7. Can glipizide cause weight gain?
Yes. Some people gain weight while taking glipizide. Eating balanced meals and exercising can help.
8. How does glipizide compare with metformin?
Metformin improves insulin sensitivity and often helps with weight. Glipizide stimulates insulin release and can cause weight gain.
9. Will I need to stop glipizide before surgery?
Often, yes. Surgeons or anesthesiologists may advise stopping it 24 hours before certain procedures. Always follow medical instructions.
10. How do I treat a severe hypoglycemia episode?
If you are conscious, consume quick sugar (glucose tablets, soda, or juice). If unconscious, someone should give glucagon and call emergency services.
References
– American Diabetes Association. Standards of Medical Care in Diabetes. https://care.diabetesjournals.org/
– U.S. Food and Drug Administration. Glipizide Label. https://www.accessdata.fda.gov/drugsatfda_docs/label/2015/018972s036lbl.pdf
– National Institute for Health and Care Excellence (NICE). Type 2 diabetes in adults: management. https://www.nice.org.uk/guidance/ng28
– UpToDate. Sulfonylureas for type 2 diabetes. (Subscription required) https://www.uptodate.com/contents/search
– Mayo Clinic. Glipizide ( (Incomplete: max_output_tokens)