- Introduction
- What Is Insulin Glargine?
- Why Dosage Matters
- Starting Dosage Guidelines
- Type 1 Diabetes
- Type 2 Diabetes
- Children and Adolescents
- Titration Strategies and Algorithms
- Simple Titration Method
- More Aggressive Titration
- Basal-Bolus Adjustments
- Timing of Administration
- Once-Daily Dosing
- Switching Injection Time
- Administration Technique
- Injection Devices
- Injection Sites and Rotation
- Step-by-Step Injection
- Mixing and Compatibility
- Storage and Handling
- Monitoring and Targets
- Glycemic Targets
- Glucose Monitoring Frequency
- Managing Hypoglycemia
- Recognize Symptoms
- Treatment and Prevention
- Special Populations
- Elderly Patients
- Pregnancy
- Renal and Hepatic Impairment
- Switching Between Basal Insulins
- Switching From NPH
- Switching From Other Long-Acting Insulins
- Combining With Oral Medications
- Adherence and Lifestyle Integration
- Addressing Injection Anxiety
- Meal Planning and Activity
- Common Side Effects and How to Manage Them
- Injection Site Reactions
- Weight Gain
- Troubleshooting Unstable Control
- Persistent Hyperglycemia
- Variable Day-to-Day Glucose
- Patient Education Checklist
- Cost, Access, and Affordability
- Recent Advances and Future Directions
- Practical Quick Reference Table
- Key Takeaways
- Frequently Asked Questions (FAQs)
- 1. How long does it take for insulin glargine to reach steady effect?
- 2. Can I split the daily dose into two injections?
- 3. What should I do if I miss a dose?
- 4. Is insulin glargine safe during breastfeeding?
- 5. How do I convert from vials to pens?
- 6. Can alcohol affect insulin glargine action?
- 7. What if I develop skin lumps at injection sites?
- 8. Can I use insulin glargine with a pump?
- 9. Does insulin glargine interact with other drugs?
- 10. How should I adjust insulin during illness?
- References
Introduction
Insulin Glargine Dosage remains a central topic for people managing diabetes. Many patients and clinicians seek clear, practical guidance. This article shares exclusive best practices based on clinical evidence and real-world use.
We focus on safe dosing, titration strategies, administration tips, and patient-centered adjustments. Consequently, readers will learn how to optimize therapy and reduce risks like hypoglycemia.
What Is Insulin Glargine?
Insulin glargine is a long-acting basal insulin. It mimics the body’s steady background insulin release. Doctors often prescribe it for type 1 and type 2 diabetes.
The medication forms microprecipitates under the skin. This property yields a slow, even release for up to 24 hours. As a result, it provides stable fasting glucose control.
Why Dosage Matters
Correct Insulin Glargine Dosage balances glucose control and safety. Too little leads to high blood sugar and long-term complications. Too much raises the chance of hypoglycemia.
Moreover, dosing affects daily routines and quality of life. Proper dosing simplifies glucose management. Therefore, patients can maintain predictable eating and activity patterns.
Starting Dosage Guidelines
Type 1 Diabetes
For adults with type 1 diabetes, clinicians often start with a total insulin dose of 0.5 to 0.8 units/kg/day. Doctors typically divide this dose between basal and bolus insulin. As a rule, they assign about 40% to 50% of the total daily dose to insulin glargine.
For example, a 70 kg adult may start with 35 to 40 units of basal insulin. Clinicians then tailor bolus doses around meals. They adjust both types based on glucose readings.
Type 2 Diabetes
For insulin-naïve adults with type 2 diabetes, start with 10 units per day or 0.1 to 0.2 units/kg/day. Clinicians choose the lower end for frail or elderly patients. Then they titrate based on fasting blood glucose.
Many clinicians prefer starting with a fixed low dose. Next, they increase the dose by 2 to 4 units every 3 days until fasting glucose targets reach. This gradual approach limits hypoglycemia.
Children and Adolescents
Pediatric dosing requires careful adjustment. Clinicians base doses on weight and insulin sensitivity. They often use a starting range of 0.2 to 0.6 units/kg/day for total insulin.
Endocrinologists split the total dose between basal and bolus insulin. Then they change the basal insulin according to growth and activity. Regular monitoring helps avoid low or high blood sugar.
Titration Strategies and Algorithms
Simple Titration Method
A simple algorithm increases or decreases insulin glargine by 2 to 4 units. Patients adjust every 3 to 7 days based on fasting glucose averages. For example, if fasting glucose averages above goal, increase the dose.
Conversely, if fasting glucose falls below the target, reduce the dose to prevent hypoglycemia. This method works well for primary care and patient self-titration programs.
More Aggressive Titration
Clinicians may use a tighter schedule for patients needing faster control. They might increase by 4 units every 3 days, with closer monitoring. However, they must weigh the higher hypoglycemia risk.
Often, providers use this method in structured care settings. They include frequent glucose testing and patient education.
Basal-Bolus Adjustments
When you use basal-bolus therapy, titrate the basal insulin to fasting glucose. Then adjust mealtime insulin for postprandial spikes. This two-step approach isolates basal needs from bolus needs.
Practically, clinicians change basal doses first. After basal control improves, they correct bolus doses for meal times. This strategy simplifies the titration process.
Timing of Administration
Once-Daily Dosing
Insulin glargine typically requires once-daily injection. Patients inject it at the same time each day for steady coverage. Many choose bedtime or the morning based on lifestyle.
Consistent timing reduces glucose variability. Therefore, patients achieve steadier fasting glucose and fewer nocturnal lows.
Switching Injection Time
You can change the injection time if needed. Do this gradually and monitor glucose closely. For example, move injection 1 to 2 hours earlier or later per day until you reach the new schedule.
Clinicians recommend monitoring fasting and pre-meal glucose during the change. That way, they detect any dose adjustments needed.
Administration Technique
Injection Devices
Insulin glargine comes in pen devices and vials for syringes. Pens improve dosing accuracy and convenience. Many patients prefer pens for portability and ease of use.
Choose a device that fits patient preferences and abilities. Also, provide training on device use to ensure proper dosing.
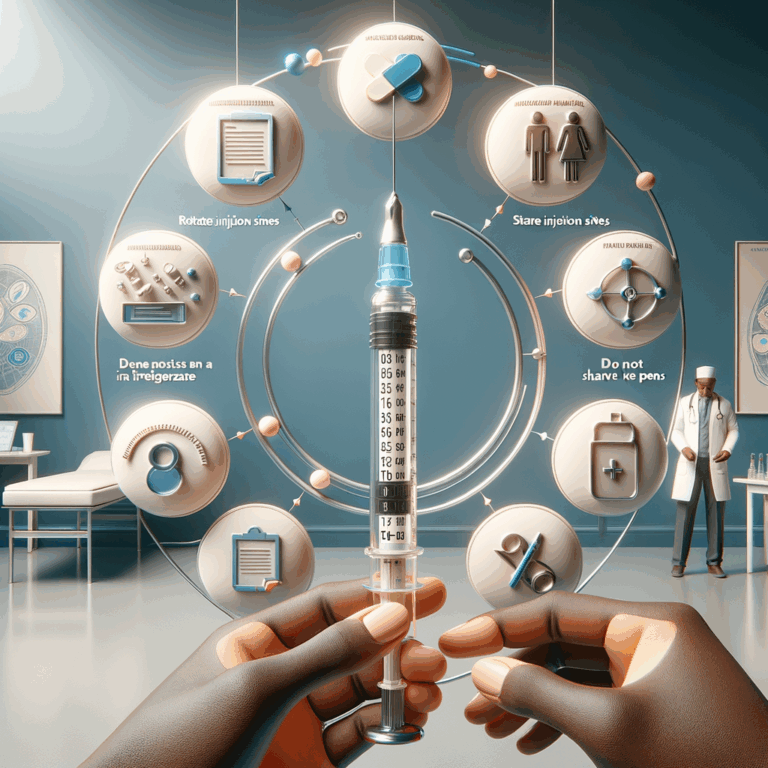
Injection Sites and Rotation
Common injection sites include the abdomen, thigh, and upper arm. The abdomen gives faster absorption and more consistent action. However, rotation remains crucial.
Rotate within the same region to maintain consistent absorption. Avoid injecting into lipohypertrophy or scarred tissue. That tissue alters insulin uptake and can lead to unpredictable glucose levels.
Step-by-Step Injection
– Clean the injection site with soap and water. Alcohol is optional unless site is visibly dirty.
– Pinch a small skin fold if using a syringe or the needle requires it.
– Insert the needle at 90 degrees for adults. Use 45 degrees for very thin patients.
– Inject the dose slowly and wait 5 to 10 seconds before removing the needle.
– Dispose of needles safely in a sharps container.
These steps reduce dosing errors and injection discomfort. They also minimize local tissue issues.
Mixing and Compatibility
Insulin glargine should not mix with short-acting insulins in the same syringe. Mixing alters its release profile and stability. Therefore, inject the basal insulin separately.
Do not mix insulin glargine with other insulins in the same vial or pen. Use separate injections to avoid destabilizing the formulation.
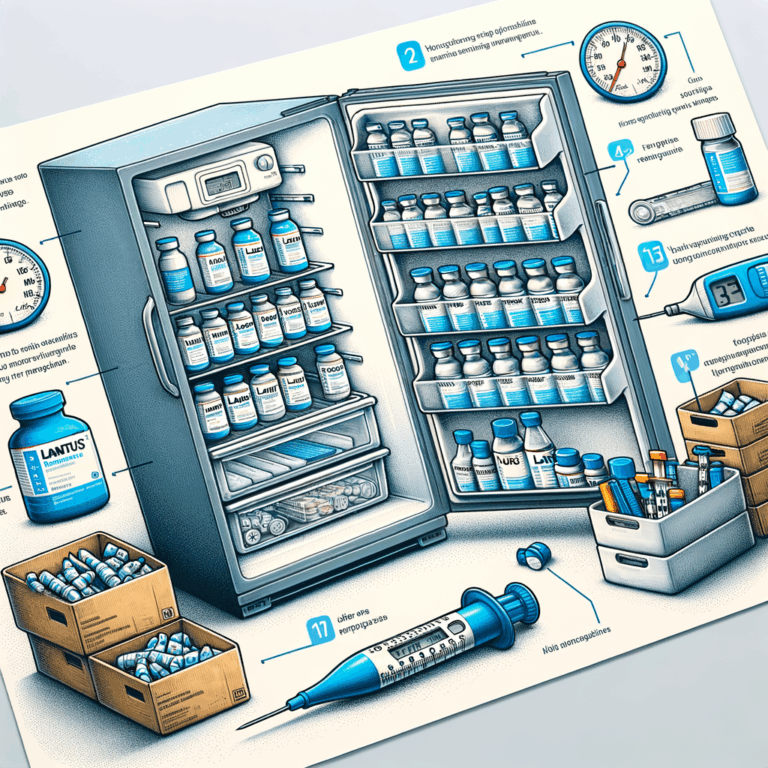
Storage and Handling
Store unopened insulin glargine in the refrigerator between 2°C and 8°C (36°F and 46°F). Do not freeze it. Keep it away from direct sunlight and high heat.
Once in use, most pens and vials can remain at room temperature. Discard them after the manufacturer’s recommended period. This period commonly ranges from 28 to 30 days. Always confirm specifics on the product label.
Monitoring and Targets
Glycemic Targets
Individualize glucose targets based on age and comorbidities. For many nonpregnant adults, aim for an A1C below 7%. Fasting glucose targets often fall between 80 and 130 mg/dL.
Older adults or those with limited life expectancy may need higher A1C targets. Discuss goals with the treating clinician.
Glucose Monitoring Frequency
At baseline and during titration, monitor fasting glucose daily. Later, test several times weekly once stabilized. However, increase testing during illness, dose changes, or when symptoms appear.
Continuous glucose monitoring (CGM) offers richer data. Use CGM trends to refine dosing and timing decisions.
Managing Hypoglycemia
Recognize Symptoms
Common hypoglycemia signs include sweating, tremor, palpitations, and confusion. Some people experience hunger and irritability. Teach patients to recognize and act on early signs.
Prompt recognition prevents severe events. Encourage patients to carry quick sources of glucose.
Treatment and Prevention
Treat mild hypoglycemia with 15 grams of fast-acting carbs. Recheck glucose after 15 minutes. Repeat treatment if glucose remains low.
To prevent recurrent lows, review meal timing, activity, and dosing. Consider reducing insulin glargine by 10% to 20% if recurrent nocturnal hypoglycemia occurs. Always discuss dose changes with a clinician.
Special Populations
Elderly Patients
Older adults often have reduced renal function and unpredictable eating. Start with lower doses and titrate slowly. Aim for more relaxed glucose targets to reduce hypoglycemia risk.
Use simpler regimens when possible. Simplified dosing improves adherence and safety.
Pregnancy
Insulin glargine crosses the placenta minimally. Despite this, many guidelines recommend short-acting and intermediate insulins during pregnancy. Some clinicians continue glargine when benefits outweigh risks.
Pregnant patients need frequent monitoring and dose changes. Coordinate care with an obstetrician and endocrinologist.
Renal and Hepatic Impairment
Renal impairment increases insulin sensitivity and decreases clearance. Therefore, reduce starting doses in patients with kidney disease. Monitor glucose closely and adjust often.
Advanced liver disease similarly reduces insulin metabolism. Titrate carefully and expect lower insulin requirements.
Switching Between Basal Insulins
Switching From NPH
When switching from NPH to insulin glargine, many clinicians use a 1:1 conversion. However, reduce the dose by 10% to 20% if hypoglycemia history exists. Monitor fasting glucose and adjust as needed.
Glargine provides more stable coverage and less nocturnal hypoglycemia. Communicate expectations to patients about different action profiles.
Switching From Other Long-Acting Insulins
When changing between basal analogs, use close to a 1:1 conversion. Still, individual response varies. Hence, schedule a review after 3 to 7 days.
Pay attention to timing differences. Some long-acting insulins have slightly different durations and peaks. Adjust the injection time and dose accordingly.
Combining With Oral Medications
Insulin glargine often complements oral antidiabetic drugs. For example, clinicians add it to metformin when oral therapy fails. Combining therapies can improve glycemic control.
Stop or adjust sulfonylureas when adding basal insulin if hypoglycemia becomes an issue. DPP-4 inhibitors and SGLT2 inhibitors can remain in many regimens. Coordinate medication changes with a clinician.
Adherence and Lifestyle Integration
Addressing Injection Anxiety
Many patients fear needles. Provide demonstrations and practice with placebo pens. Encourage the use of shorter needles and distraction techniques.
Education and support reduce anxiety and improve adherence. Patients who feel confident inject more consistently.
Meal Planning and Activity
Encourage consistent meal timing relative to basal insulin. Regular eating patterns reduce glucose variability. Likewise, prepare for exercise by adjusting carbohydrate intake or insulin dosing.
Teach patients how activity affects insulin sensitivity. Active days may require lower doses or extra carbs.
Common Side Effects and How to Manage Them
Injection Site Reactions
Mild redness or swelling can occur. Usually, these reactions resolve quickly. Rotate sites to minimize local reactions and lipohypertrophy.
If reactions persist or worsen, reassess technique and rule out allergy. In rare cases, switch the formulation after consulting a clinician.
Weight Gain
Insulin therapy can cause modest weight gain. Encourage dietary adjustments and increase physical activity. Consider combining insulin with lifestyle and adjunctive medications when appropriate.
Discuss expectations clearly with patients. Proper counseling helps maintain motivation.
Troubleshooting Unstable Control
Persistent Hyperglycemia
First, confirm proper injection technique and device function. Next, evaluate adherence, meal patterns, and concurrent illnesses. Consider increasing the basal dose if fasting glucose stays high.
If postprandial glucose remains elevated, adjust mealtime insulin or non-insulin agents. Always rule out factors like steroid use or infections.
Variable Day-to-Day Glucose
Day-to-day variability often stems from inconsistent meal timing or exercise. Review lifestyle routines and injection site rotation. Also, check for errors in syringe or pen use.
Continuous glucose monitoring can identify patterns and help fine-tune therapy.
Patient Education Checklist
Use this checklist during patient counseling:
– Understand the purpose of basal insulin.
– Learn correct injection technique and site rotation.
– Keep a log of fasting glucose values.
– Know hypoglycemia signs and treatments.
– Store insulin correctly and check expiration dates.
– Carry quick carbohydrates and a glucagon kit if prescribed.
– Schedule regular follow-up and A1C testing.
This set of actions empowers patients and encourages safe self-management.
Cost, Access, and Affordability
Insulin glargine can be costly without insurance. Many manufacturers offer patient assistance programs. Also, some clinics use biosimilar or lower-cost options to improve access.
Discuss cost concerns openly. Clinicians can help find programs, coupons, or alternative therapies that maintain safety.
Recent Advances and Future Directions
Manufacturers and researchers keep improving basal insulin options. Newer formulations aim for longer duration and less variability. Biosimilars and concentrated forms also expand choices.
In the future, better-aligned dosing algorithms and smart pens could simplify dosing. Meanwhile, research on combination therapies continues.
Practical Quick Reference Table
| Situation | Starting Dose | Titration |
|---|---|---|
| Type 1 Adult | 0.5–0.8 units/kg/day total; basal 40–50% | Adjust basal based on fasting glucose |
| Type 2 Insulin-naïve | 10 units/day or 0.1–0.2 units/kg/day | Increase 2–4 units every 3–7 days to target |
| Elderly/Frail | Lower starting dose, e.g., 0.1 units/kg | Titrate slowly; higher glucose targets |
| Renal Impairment | Reduce starting dose by 20–30% | Adjust frequently based on readings |
Key Takeaways
Insulin glargine provides stable basal insulin coverage. Accurate dosing improves control and reduces risks. Start conservatively and titrate based on fasting glucose.
Educate patients on technique, rotation, and hypoglycemia management. Tailor dosing for age, comorbidities, and lifestyle. Use monitoring data to guide adjustments.
Now, let’s answer common questions you may still have.
Frequently Asked Questions (FAQs)
1. How long does it take for insulin glargine to reach steady effect?
Insulin glargine reaches near-steady action within 2 to 4 days. However, visible clinical effects may require a week of consistent dosing. Monitor fasting glucose to confirm stability.
2. Can I split the daily dose into two injections?
You can split doses when needed, though manufacturers design it for once daily use. Some patients benefit from twice-daily dosing if they have uneven coverage. Discuss this with your clinician.
3. What should I do if I miss a dose?
Inject the missed dose as soon as you remember, provided it is not close to the next scheduled dose. If it is near the next dose, skip the missed dose. Avoid doubling doses to catch up.
4. Is insulin glargine safe during breastfeeding?
Limited data suggest minimal transfer into breast milk. Many clinicians consider glargine acceptable during breastfeeding. Still, consult your healthcare provider for personalized advice.
5. How do I convert from vials to pens?
Conversion is typically 1:1 for dose strength. Ensure you understand pen device steps and needle sizes. Observe initial doses to confirm correct delivery and absorption.
6. Can alcohol affect insulin glargine action?
Alcohol can increase insulin sensitivity and raise hypoglycemia risk. Monitor glucose closely when drinking alcohol, and consider reducing dose or consuming carbs with alcohol.
7. What if I develop skin lumps at injection sites?
Lumps often result from lipohypertrophy due to repeated injections. Stop injecting into those areas and rotate sites. Have lumps checked by a clinician if they persist.
8. Can I use insulin glargine with a pump?
Insulin glargine is not designed for pump use. Pumps require rapid-acting insulin formulations. Do not use basal analogs in pumps without explicit medical guidance.
9. Does insulin glargine interact with other drugs?
Many medications affect blood sugar and insulin needs. Corticosteroids, beta-blockers, and certain psychiatric drugs can change requirements. Review medication lists with your clinician.
10. How should I adjust insulin during illness?
Illness often raises blood glucose. Maintain hydration, monitor glucose frequently, and follow sick-day rules. You may need extra short-acting insulin. Contact your care team for guidance.
References
– American Diabetes Association. Standards of Care in Diabetes—2025. https://diabetesjournals.org/care/ (Please refer to the latest ADA Standards for detailed guidance)
– U.S. Food and Drug Administration. Lantus (insulin glargine) prescribing information. https://www.accessdata.fda.gov/drugsatfda_docs/label/2015/020150s051lbl.pdf
– Nathan, D. M., Buse (Incomplete: max_output_tokens)