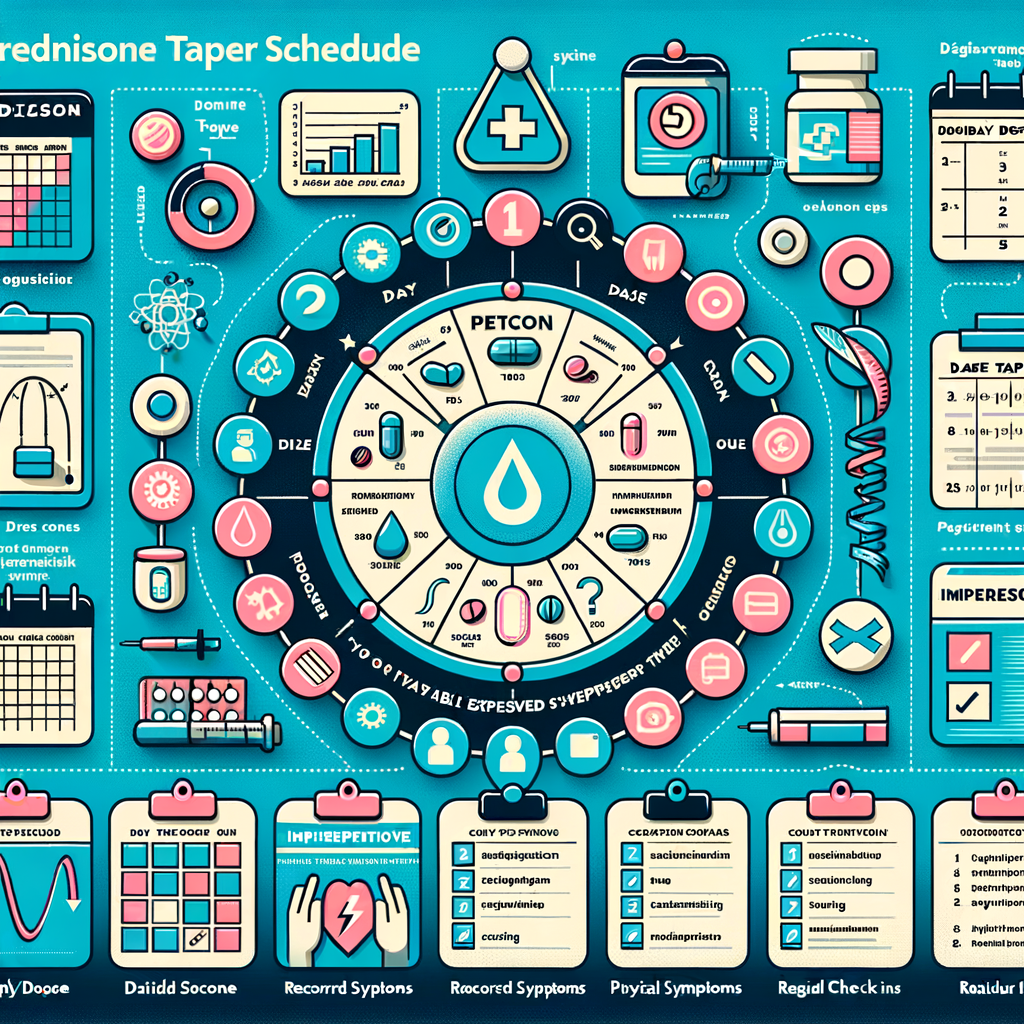
- Why a Prednisone Taper Schedule Matters
- How Prednisone Affects Your Body
- Who Needs a Taper and When
- Principles of a Safe Prednisone Taper Schedule
- Common Tapering Methods
- Linear Taper
- Percentage Taper
- Plateau Then Rapid Drop
- Sample Prednisone Taper Schedule Templates
- Short Course (≤10 days)
- Moderate Course (2–4 weeks)
- Long Course (>4 weeks)
- Adjusting the Taper Based on Symptoms
- Steroid Withdrawal vs. Disease Flare
- Special Considerations for Certain Conditions
- Rheumatologic Conditions
- Pulmonary Conditions
- Gastrointestinal Conditions
- How to Reduce Side Effects During Tapering
- Diet and Lifestyle Tips
- Bone Health
- Medication Interactions to Watch For
- Monitoring During a Prednisone Taper Schedule
- When to Seek Emergency Care
- How Long Does It Take for Adrenal Function to Return?
- Pediatric and Geriatric Considerations
- Using Alternate-Day Therapy
- Patient Tips for a Smooth Taper
- Myths and Misconceptions About Tapering
- Practical Tapering Example Table
- Role of Other Therapies During Taper
- Travel, Procedures, and Steroid Coverage
- Insurance and Cost Considerations
- Emotional and Psychological Effects
- Long-Term Follow-up After Taper
- Conclusion: Safe Tapering Starts with Planning
- Frequently Asked Questions (FAQs)
- 1. How quickly can I stop prednisone without problems?
- 2. Can I taper prednisone on my own?
- 3. What are signs of adrenal insufficiency during a taper?
- 4. Does tapering prevent all side effects?
- 5. How does stress affect my taper?
- 6. Can I take herbal supplements to help taper?
- 7. Will prednisone tapering affect my diabetes?
- 8. How do I manage insomnia during tapering?
- 9. Is a steroid card necessary?
- 10. What if my disease flares during taper?
- References
Why a Prednisone Taper Schedule Matters
Prednisone works fast to reduce inflammation and suppress the immune system. However, stopping prednisone suddenly can cause withdrawal and harm. Therefore, a proper prednisone taper schedule helps your body adjust. It reduces side effects and prevents relapse of symptoms.
Doctors prescribe tapering to restore your body’s natural cortisol production. Cortisol is a hormone your adrenal glands make. Long prednisone use can suppress cortisol production. Thus, tapering allows your adrenal glands to resume normal function slowly.
How Prednisone Affects Your Body
Prednisone mimics cortisol and dampens immune response. Consequently, it controls symptoms in many inflammatory and autoimmune conditions. Still, its action affects multiple organs, metabolism, and mood.
Short-term side effects include insomnia, increased appetite, and mood changes. Long-term use can cause weight gain, osteoporosis, high blood pressure, and diabetes. Because of these risks, clinicians aim to use the lowest effective dose for the shortest time.
Who Needs a Taper and When
Not everyone needs a taper after prednisone. Short courses, usually under 7 to 10 days, often require no taper. Doctors avoid tapering when treatment is brief and doses are low. Conversely, people on prednisone for weeks or months need a taper.
Patients on daily doses above physiologic levels, typically greater than 7.5 mg, should taper slowly. Additionally, those taking alternate-day therapy or multiple steroid bursts may need a tailored approach. Always consult your healthcare provider before changing doses.
Principles of a Safe Prednisone Taper Schedule
A good taper follows a few core principles. First, lower doses gradually to reduce withdrawal risk. Second, monitor symptoms closely and adjust the pace if needed. Third, maintain the lowest effective dose to control the underlying disease.
Moreover, tapering requires flexibility. Some people tolerate faster reduction, while others need slower change. Your doctor will consider disease activity, duration of steroid use, and other medications when designing a taper schedule.
Common Tapering Methods
There are several taper strategies used in practice. Each method suits different situations. Below are typical approaches.
Linear Taper
In a linear taper, you reduce the dose by a fixed amount regularly. For example, you may decrease prednisone by 5 mg every week. This method works when initial doses are moderate.
Linear tapering offers predictability. Yet, it may be too fast for long-term users. Therefore, clinicians monitor symptoms closely and modify the plan if needed.
Percentage Taper
Percentage taper reduces the dose by a set fraction, such as 10% to 20%, every week. This approach slows reduction as doses get smaller. It works well when patients have taken prednisone for many weeks.
Because smaller doses matter more physiologically, percentage taper can feel safer. Still, you must watch for withdrawal symptoms and disease flare during the process.
Plateau Then Rapid Drop
Sometimes clinicians lower to a moderate dose and hold there briefly. Then they taper more quickly. This approach helps control disease activity before a sharper reduction.
However, a sudden final drop can risk adrenal insufficiency if not timed correctly. Therefore, doctors reserve this method for selected cases under close supervision.
Sample Prednisone Taper Schedule Templates
Below are common tapered schedules. Use them only as examples. Your provider will create a personalized plan.
Short Course (≤10 days)
– 40 mg daily for 3 days
– 20 mg daily for 3 days
– 10 mg daily for 4 days
This short course tapers modestly and often avoids adrenal suppression. Most patients need no further taper afterwards.
Moderate Course (2–4 weeks)
– 40 mg daily for 7 days
– 30 mg daily for 5 days
– 20 mg daily for 5 days
– 10 mg daily for 5 days
This linear approach reduces dose steadily. It suits moderate-term users who took higher doses.
Long Course (>4 weeks)
– 60 mg daily for 2 weeks
– 40 mg daily for 2 weeks
– 30 mg daily for 2 weeks
– 20 mg daily for 2 weeks
– 10 mg daily for 2 weeks
– 5 mg daily for 2 weeks
– 2.5 mg daily for 2 weeks then stop
This example shows a slow taper for those on high-dose long-term therapy. It helps the adrenal glands recover gradually.
Adjusting the Taper Based on Symptoms
You must report new symptoms during tapering. Symptoms can signal either disease flare or steroid withdrawal. Distinguishing the two is critical for safe management.
Common withdrawal signs include fatigue, weakness, nausea, and joint pain. Fever, rash, or clear disease-specific signs suggest relapse. If you develop severe symptoms, contact your provider promptly. They may pause reduction or increase the dose temporarily.
Steroid Withdrawal vs. Disease Flare
Steroid withdrawal results from low cortisol levels. It may cause general malaise and low blood pressure. In contrast, a disease flare shows symptoms tied to the underlying condition. For instance, asthma flare includes wheezing and shortness of breath.
Your doctor may use blood tests or clinical judgment to differentiate the two. Sometimes, a trial increase in prednisone clarifies the cause. Therefore, maintain open communication and document symptoms during the taper.
Special Considerations for Certain Conditions
Different diseases require tailored tapers. Autoimmune disorders, asthma, and inflammatory bowel disease each pose unique risks. So clinicians modify schedules based on disease activity.
For instance, lupus flares can be severe and unpredictable. Doctors often taper slowly and monitor labs. Similarly, asthma patients may need inhaled therapies to compensate when lowering oral steroids.
Rheumatologic Conditions
Patients with rheumatoid arthritis or polymyalgia rheumatica benefit from slow tapers. These diseases can flare if steroids fall too fast. Meanwhile, disease-modifying drugs can allow earlier reductions.
Therefore, clinicians often coordinate steroid taper with increased or adjusted disease-modifying therapy. This strategy lowers steroid exposure while maintaining control.
Pulmonary Conditions
Asthma and COPD patients need a cautious approach. Short bursts for exacerbations usually resolve without taper. But chronic steroid therapy demands slow reduction.
Use inhaled steroids and bronchodilators to reduce oral prednisone. Pulmonary function tests can guide tapering in these patients.
Gastrointestinal Conditions
Inflammatory bowel diseases, such as Crohn’s and ulcerative colitis, require careful taper. Relapse can lead to hospitalizations. Gastroenterologists often taper steroids slowly while introducing maintenance meds.
Additionally, infectious complications can mimic flare. Thus, monitor stool tests and infection markers during taper.
How to Reduce Side Effects During Tapering
You can manage many steroid side effects proactively. Lifestyle changes and medications help reduce risk. For example, bone health and blood sugar require special attention.
First, maintain a balanced diet and exercise regularly. Calcium and vitamin D support bone health. Second, monitor blood pressure and glucose levels. Third, avoid smoking and limit alcohol.
Doctors may prescribe bisphosphonates for bone protection. They may also adjust diabetes medications temporarily. Work with your provider to create a comprehensive plan.
Diet and Lifestyle Tips
– Eat a diet rich in lean protein, vegetables, and whole grains.
– Limit salt intake to help prevent fluid retention.
– Exercise weight-bearing activities three times weekly.
– Practice good sleep hygiene to counter insomnia.
These small changes reduce many prednisone-related risks. They also help your body regain balance during tapering.
Bone Health
Steroids speed bone loss, especially with long use. Consequently, doctors often check bone density before or during long-term therapy. They also recommend calcium (1,000–1,200 mg) and vitamin D (800–1,000 IU) daily.
If bone density is low, clinicians may start bisphosphonates. These drugs protect against fractures. Always ask your doctor which bone-protective option fits you best.
Medication Interactions to Watch For
Prednisone interacts with several medicines. These interactions can alter drug levels or increase side effects. Always tell providers about all medications, supplements, and herbal remedies.
Common interactions include certain antifungals, anticonvulsants, and blood thinners. For example, itraconazole can raise steroid levels, increasing side effects. Meanwhile, enzyme-inducing drugs like phenytoin may lower steroid effectiveness.
Your provider will adjust doses or suggest alternatives when needed. Pharmacists can also review interactions and offer guidance.
Monitoring During a Prednisone Taper Schedule
Regular monitoring helps catch problems early. Your doctor may order blood tests, bone density scans, or other studies. They will track blood pressure, glucose, and signs of infection.
Keep a symptom diary during the taper. Note energy levels, appetite changes, mood shifts, and disease-specific signs. Bring this record to appointments. It helps clinicians decide whether to speed up, slow, or pause the taper.
When to Seek Emergency Care
Certain symptoms require urgent evaluation. Seek emergency care if you have severe weakness, dizziness, fainting, or low blood pressure. Also seek help for chest pain, severe shortness of breath, or sudden high fever.
These signs may indicate adrenal crisis or a severe disease flare. Prompt treatment can be life-saving. Therefore, do not delay getting emergency help if symptoms escalate quickly.
How Long Does It Take for Adrenal Function to Return?
Adrenal recovery time varies widely. It depends on dose, duration, and individual factors. Some people recover in weeks; others take months or longer.
Doctors can test adrenal function with ACTH stimulation tests. These tests determine if your body makes enough cortisol. Providers use results to guide final weaning steps and to decide on taper pace.
Pediatric and Geriatric Considerations
Children and older adults require special care. Kids metabolize steroids differently and may need different schedules. Growth suppression concerns make slow tapering and careful monitoring essential.
Older adults face higher risks of osteoporosis, diabetes, and infections. They often need bone protection and closer monitoring. Both groups benefit from a tailored, cautious taper plan.
Using Alternate-Day Therapy
Alternate-day therapy reduces side effects in some chronic conditions. Patients take a higher dose every other morning instead of daily lower doses. This schedule lets the adrenal gland recover on off days.
However, alternate-day therapy works best for certain diseases and stable patients. It may not suit acute flares or rapidly changing conditions. Your clinician will decide if it fits your situation.
Patient Tips for a Smooth Taper
Keep a medicine calendar and record each dose. This practice prevents missed or duplicated doses. Also, carry a medical alert card stating you use steroids.
Communicate symptom changes immediately to your healthcare team. Ask for written taper plans and emergency instructions. Finally, keep follow-up appointments consistently.
Myths and Misconceptions About Tapering
Many myths surround steroid tapering. One myth says you must always taper slowly regardless of duration. In reality, short courses rarely need taper. Another myth claims tapering prevents all side effects. In truth, tapering reduces withdrawal but does not prevent all adverse effects.
You should also know that supplements or “detox” regimens cannot replace medical tapering. Always follow medical guidance and avoid unproven remedies.
Practical Tapering Example Table
Below is a practical example for someone on a prolonged prednisone course. Use this table only for understanding. Your doctor will provide the exact plan.
| Weeks on Steroids | Starting Dose | Taper Plan |
|---|---|---|
| 2–4 weeks | 20–40 mg | Reduce by 5–10 mg every 3–7 days |
| 1–3 months | 20–60 mg | Reduce by 5–10 mg every 1–2 weeks, then smaller steps at low doses |
| >3 months | >40 mg | Slow taper: reduce by 5–10 mg every 2–4 weeks; switch to percent reductions near low doses |
Role of Other Therapies During Taper
Doctors often introduce steroid-sparing agents during taper. These drugs reduce reliance on prednisone. Examples include methotrexate, azathioprine, and biologics. They help maintain disease control.
Physical therapy, counseling, and lifestyle interventions also support recovery. For instance, exercise can counter weight gain and muscle weakness. Mental health support helps with mood changes and sleep problems.
Travel, Procedures, and Steroid Coverage
If you travel or undergo surgery during a taper, tell providers about your steroid use. Stressful events require higher steroid doses temporarily. Surgeons often give “stress-dose” steroids during major procedures.
Also, carry documentation proving your prednisone use. This record helps ER staff manage adrenal insufficiency risks. Plan ahead and discuss any upcoming travel or surgeries with your doctor.
Insurance and Cost Considerations
Steroid-sparing agents and monitoring tests can raise costs. Talk to your medical team and insurance company early. They may approve generic drugs or alternative therapies to lower expenses.
Medication assistance programs and patient support organizations can also help. Ask your provider or pharmacist about available resources.
Emotional and Psychological Effects
Prednisone can cause mood swings, anxiety, and insomnia. These effects may intensify during tapering. Recognize emotional changes as part of the process.
Seek support from family, friends, or mental health professionals. Simple strategies like sleep hygiene and relaxation techniques help. If mood changes worsen, consult your provider about medication adjustments.
Long-Term Follow-up After Taper
Even after stopping prednisone, follow-up matters. Your doctor will reassess the underlying condition and monitor for relapse. They may order periodic blood tests and bone density screening.
If adrenal testing shows incomplete recovery, your physician will guide further steps. Some patients need ongoing low-dose steroids for months. Therefore, see your provider regularly until they clear you.
Conclusion: Safe Tapering Starts with Planning
A prednisone taper schedule requires planning, monitoring, and flexibility. Work closely with your healthcare team to reduce risks. Report symptoms promptly and follow medical advice.
Remember, tapering protects your adrenal health and helps prevent relapse. With the right approach, you can minimize side effects and regain control.
Frequently Asked Questions (FAQs)
1. How quickly can I stop prednisone without problems?
You can often stop prednisone abruptly if you took it for less than 7 to 10 days. Longer courses require tapering to avoid withdrawal. Always check with your prescriber first.
2. Can I taper prednisone on my own?
No. You should not adjust prednisone without medical guidance. Your doctor knows your disease and risks. Improper tapering can lead to adrenal crisis or disease flare.
3. What are signs of adrenal insufficiency during a taper?
Watch for severe fatigue, dizziness, fainting, nausea, and low blood pressure. If you notice these, seek medical care immediately.
4. Does tapering prevent all side effects?
No. Tapering mainly prevents withdrawal and supports adrenal recovery. It does not eliminate other steroid side effects like weight gain or osteoporosis.
5. How does stress affect my taper?
Stress increases your body’s demand for cortisol. During illness, surgery, or severe stress, you may need temporary higher steroid doses. Always inform your doctor about such events.
6. Can I take herbal supplements to help taper?
Avoid relying on herbal supplements to replace medical tapering. Some supplements interact with prednisone. Consult your provider before starting any new supplement.
7. Will prednisone tapering affect my diabetes?
Yes. Prednisone can raise blood sugar. During taper, your diabetes medication may need adjustments. Monitor glucose closely and follow your diabetes care plan.
8. How do I manage insomnia during tapering?
Practice sleep hygiene, reduce stimulants, and follow a bedtime routine. If insomnia persists, discuss sleep aids with your clinician. Avoid over-the-counter sleep products without advice.
9. Is a steroid card necessary?
Yes. A steroid card or medical alert card helps emergency providers know you use steroids. It guides proper emergency and surgical care.
10. What if my disease flares during taper?
Contact your healthcare provider immediately. They may increase the prednisone dose temporarily or adjust other therapies. Do not resume previous doses without medical direction.
References
– UpToDate. “Glucocorticoid withdrawal and adrenal insufficiency.” https://www.uptodate.com/contents/glucocorticoid-withdrawal-and-adrenal-insufficiency
– American College of Rheumatology. “Glucocorticoid use and bone health.” https://www.rheumatology.org/Practice-Quality/Clinical-Support/Clinical-Practice-Guidelines
– Mayo Clinic. “Prednisone (Oral Route) Side Effects.” https://www.mayoclinic.org/drugs-supplements/prednisone-oral-route/side-effects/drg-20075269
– British National Formulary. “Corticosteroids: prescribing and tapering.” https://bnf.nice.org.uk/treatment-summary/corticosteroids/
– National Institutes of Health (NIH). “Adrenal Insufficiency and Glucocorticoid Withdrawal.” https://www.ncbi.nlm.nih.gov/books/NBK279135/
Note: This article provides general information and examples. It does not replace medical advice. Always consult your healthcare provider for personalized care.